1.1a: Tissues and Bone Development (Part A)
1.1b: Tissues and Bone Development (Part B)
1.2a: The Axial Skeleton: The Skull
1.2b: The Axial Skeleton: The Vertebral Column
RANDOMLY ORDERED NOTES (1.1a,1.1b,1.2a,1.2b)
형광펜 칠한 부분은 좀 더 찾아보기
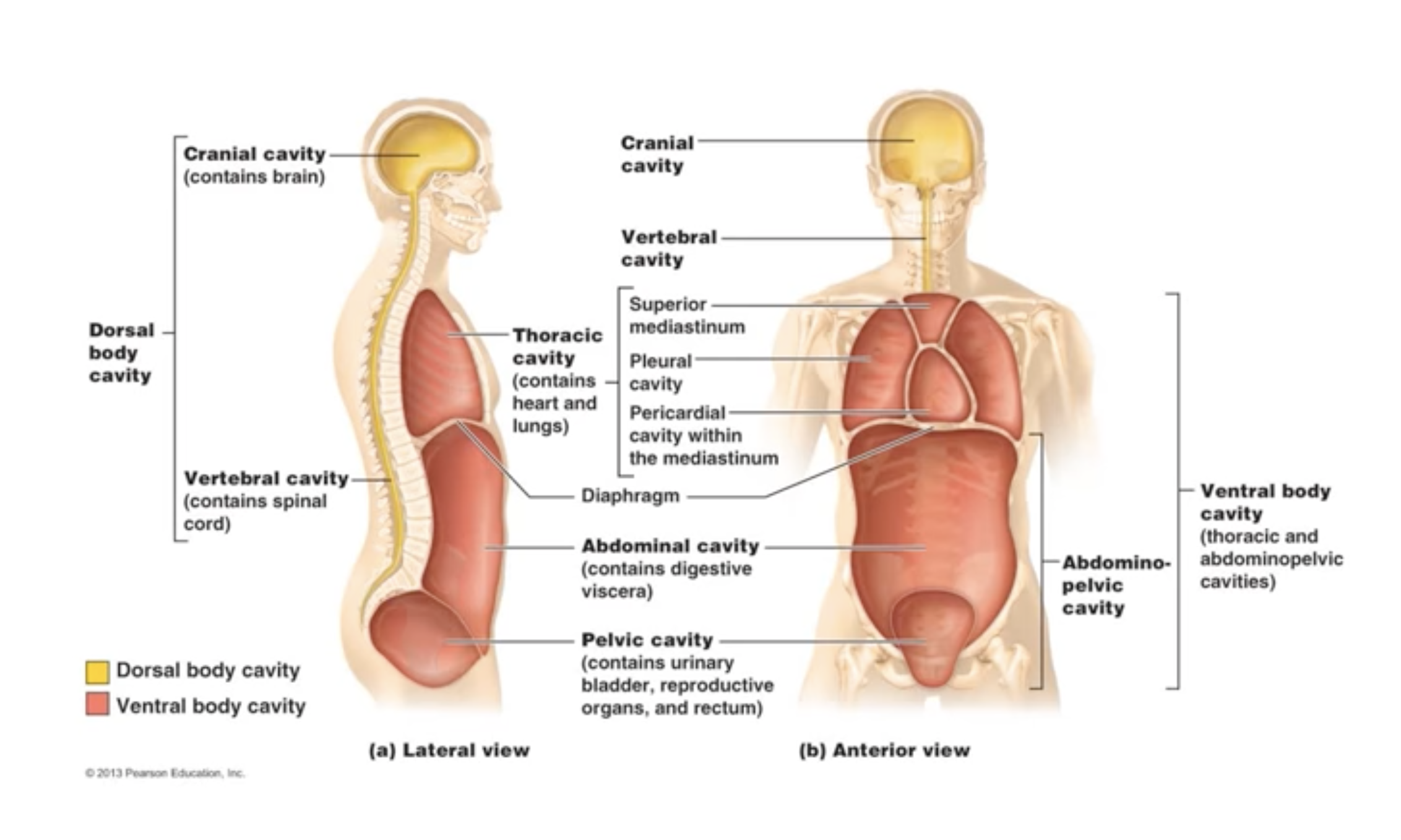
*thoracic cavity -> pleural cavities, pericardial cavity within mediastinum, superior mediastinum
*abdominal cavity -> left upper, right upper, left lower, right lower

답변들 점검 필요
1. Differntiate between the terms epiphyseal plate and epiphyseal line
Epiphyseal plate is a cartilage where ossification occurs and epiphysial line is a bone matrix which is already ossified from an epiphyseal plate. Around 25 years old, every epiphyseal plate in bones turns into epiphyseal line.
Estrogen and testosterone release at puberty initiates closure of the epiphyseal plates.
2. Outline the difference between primary and secondary ossification of long bones
Before 8 weeks, Meschondyle cell produce embryonic skeleton made of hyaline cartilage and fibrous membrane. From 8weeks, primary ossification centers are formed and start to ossify. Around 12 weeks, most of the bones has well defined primary ossificarion center. At birth, most long bones are well ossified except for the epiphyses where the length development continues after birth. Around the birth, the secondary ossification appear and develop in a predictablw sequence at the epiphyseal growth plate. By 25 years old, nearly all growth plates are completely ossified and skletal growth ceases.
3. What is the difference between superior and proximal?
Superior is the term used based on transverse/ horizontal plane. Superior means upper side and inferior means lower direction of the body.
Proximal means closer to the body trunk or the joints. The opposite term of proximal is distal.
4. Outline the difference between osteoblasts and osteoclasts? Within bone tissue, where do you find them?
Osteoblasts are the bone builder. They bring calcium and other nutrients by blood vessels and ossify surrounding area into bone matrix. Osteoclasts are responsible for resorption of the bone. They chip away the bone matrix and release calcium into the blood vessels.
These cells are found on the surface of the bone. Osteoblasts are developed from osteogenic cells in the periosteum. Osteoclasts can also be found in the endosteum of the marrow cavity.
5. Review Osteoporosis and outline the physiological basis of current preventative measures
6. Compare osteomalacia and rickets. Why does rickets cause greater deformities of the skeleton?
Osteomalacia is explained with softening of bones. Bone density gets lower mostly
Osteoprosis refers to the condition of weaken bones.
If osteoprosis happens specially due to the vitamin D deficiency then it's called osteomalacia.
If the child gets poor diet on vitamin D and have difficulty in absorbing calcium, then it's called rickets.
Osteoprosis is more general term and has various factors to get that condition.
7. What are trabeculae?
Trabaculae are located in the sponge bone (cancellous bone) They are the space between the sponge bone matrix.
Red blood marrow is stored in trabaculae.
8. In a short paragraph, explain Wolff's Law
Wolff's law explains the growth in bone strength. When the
9. What is appositional growth?
Appositional growth is the bone width growth.
10. Briefly outline hormonal control of bone remodeling. Would an insufficient intake of calcium affect PTH secertion? How?
Bone remodels by appositional growth. Osteoblasts beneath the periosteum secrete bone matrix on the external bone surface, while osteoclasts on the endosteum or surface of the diaphysis resorb, or remove bone.
If we insufficiently intake calcium in our diet, PTH released from parathyroid gland stimulates osteoclasts to resorb bone releasing calcium into the blood stream. As blood concentrations of calcium rise, the stimulus for parathyroid hormone release ends.
+ Calcitonin is a hormone produced in the thyroid gland, but its affects on calcium homeostasis are negligible in humans. It does help to lower blood calcium levels temporarily, if delivered at a pharamacological dose.
11. Explain what an osteon/ Haversian system is
Osteon system includes central canal and layered bone matrix called lamella.
Central canals are filled with bundles of nerve and blood vessels.
Volkmann's canal joins one Haversian canals together, connects the blood and nerve supply of the medullary cabity to the central canals.
Osteocytes are the living cells trapped in lacunae (little islands or spaces) and they are connected with canaliculi.
Collagen fibers of lamellae running different angle make the strength toward the torsion forces.
12. Explain why an underactive parathyroid gland can lead to hypocalcaemia (low blood calcium)?
When calcium level in blood is low, Parathyroid secretes prathyroid horomones which activate osteoclasts to resorpt the bone matrix in order to release calcium into the blood vessels. As a result, bone density decreases but the calcium level can maintain its consistency. However if the parathyroid is underactive, they cannot make bone to release calcium into the blood.
13. When do secondary spinal curvatures occur?
Primary curvature(The cervical curve forms) develops when the infant is able to hold up his or her head (at three or four months) and sit upright (at nine months. Secondary curvatures (The lumbar curve forms) develop when the child begins to walk.
14. What factors can cause kyphosis and lordosis?
Lordosis (also known as swayback) is when the lower back, above the buttocks, curves inward too much, causing the child's abdomen to protrude and buttocks to stick out.
Kyphosis is when the upper spine curves too far outward, forming a hump on the upper back.

-Wolff's Law states that a bone grows and remodels in response to the demands placed on it.
If loading on a particular bone increases, the bone will remodel itself over time to become stronger to resist that sort of loading.
A bone is loaded or stressed whenever weight bears down on it or muscles contract and pull on it. Often this loading is off center and tends to bend the bone. Bending compresses the bone on one side and subjects it to tension or stretchung on the other. As result of the stress, long bones are the thickest midway along the shaft of the diaphysis, exactly where bending stresses are greatest. Both compression and tension are minimal towards the centre of the bone (hollow inside). The osteocytes respond to the pressure and release biochemical factors that initiate remodelling. Deforming a bone produces an electrical current and it is suggested that the electrical signals direct the remodelling.- this is the principle underlying some treatment devices used to speed bone healing. The skeleton is continuously subjected to both horomonal influences and mechanical forces, working together to remodel bone. The hormonal controls determine whether and when remodelling occurs in response to changing blood calcium levels, and mechanical stress determines where the remodelling occurs.
-Endochondral ossification -> long bones of the femur, humerus, radius. almost all bones below base of skull.
-Intramembranous ossification -> flat bones of the cranium, sternum
-interstitial growth : bone length grow (stops when the epiphyseal plate turns into epiphyseal line)
-appositional growth allows bones to grow in diameter. (width growth)
-epiphyseal plate is a cartilage and epiphyseal line is bone tissue
-Difference between Osteoporosis , osteomalacia
*osteoporosis 골다공증 : bone mass decreases, bone ratio(mineral, bone matrix) is normal . weakening of the bone
-> results from a combination of lowpeak bone mass, increased bone resoption, and impaired bone formation
*osteomalacia 골연화증 : ratio of bone mineral to bone matrix is low . bones not hardening .sofetning bone
-> osteomalacia only happens in adults, and when the same thing happens in children, it's called rickets.
-> more common in women and often happens during pregnancy
-> due to impaired mineralisation, usually because of severe vitamin D deficiency.
*Density of bone tissue decrease -> osteoprosis
Cartilage wears off -> osteo arthritis
-Transverse foramina is the hole in cervical vetebrae.
-Volkmann's canal joins the periosteum and haversian canal with another. It connect the blood and nerve supply of the medullary cavuty to the central canals.
-Osteocytes are the living cells hidden in the lacunae (little islands or spaces) at the junction of the lamellae. These lacunae are joined together by little canals called canaliculi
-Tubercle's bigger version is tuberosity
-Calcium level in our blood vessel
Parathyroid hormone (PTH) activates osteocytes to chip away bone matrix to release calcium into the blood vessel.
As a result, bone density decreases and the calcium level in blood vessels increases.
(Parathyroid homone, blood calcium level increases, bone desity decreases, parathyroid gland)
Calcitonin is a hormone that your thyroid gland makes and releases to help regulate calcium levels in your blood by decreasing it. Calcitonin opposes the actions of the parathyroid hormone, which is a hormone that increases your blood calcium levels.
(Calcitonin, blood calcium level decreases, bone density increases, thyroid gland)
-organic bone matrix -> bone cells, fibers,
(especially collagen fibers provide bone's flexibility and great tensile strength)
Inorganic matrix -> calcium salt
(Hardness, resist compression)
-The mesoderm layer produces the embryonic mesenchymal cells, which produce the membranes and cartilages that produce the embryonic skeleton. Before week 8 of foetal development, the embryonic skeleton is made of hylaine cartilage and fibrous membranes. Then at eight weeks of foetal age, primary ossification centres are formed and the bones start to ossify. Most long bones have well-defined primary ossification centres by 12 birth most long bones are well ossified, except for the epiphyses where length development continues long after birth. Post-natally, or after birth, the bones grow in length and size, and then remodel.
The secondary ossification centers appear around the time of birth, and develop in a predicatable sequence at the epiphyseal growth plate. They provide for long bone growth throughout childhood and adolescence. By 25 years of age nearly all growth plates are completely ossified and skeletal growth ceases.
Before 8 weeks -> bones are made of hyaline and fibrous membrane
8weeks -> primary ossification centers are formed and start to ossify
8weeks ~ 12weeks -> most long bones have well-defined except for the epiphyses where length development continues
After birth -> secondary ossification centers appear around the time of birth, and devevelop in a predictable sequence at the epiphyseal growth plate.
By 25 years old -> nearly all growth plates are ossified and skeletal growth ceases
-How can physical activities strengthen bone density?
-> osteocytes can sense the pressure/workload on the bone and respond to triggering osteoblasts to increase bone density
+
conversely when bone experiences reduce loading conditions (such as long-term bedrest)
remodeling increases
-Anatomical position 이나 교과서에 사진들은 모두 그 figure 기준이고, 보고 있는 내 기준이 아님.
모든 기준은 그 환자, 그 사진 기준임, 보고 있는 내 기준이 아님.
'Griffith college Tri3 2022 > 1016MSC (AnP)' 카테고리의 다른 글
| WEEK3 - Muscular system (1) learning contents (0) | 2022.11.04 |
|---|---|
| WEEK3 - Muscular system (1) resources + note (0) | 2022.11.04 |
| WEEK2 - Skeletal system (2) learning contents (0) | 2022.11.02 |
| WEEK1 - Skeletal system (1) learning contents (0) | 2022.10.26 |
| WEEK0 - Intro (0) | 2022.10.22 |


