Topic 1.1 Introduction and overview, The Nature of the Skeletal System and how Bones grow (WEEK 1)
Topic 1.2 The Axial Skeleton (WEEK 1)
Topic 1.3 The Appendicular Skeleton (WEEK 2)
Topic 1.4 Joints (WEEK 2)
Before class
Topic 1.1 Introduction and overview, The Nature of the Skeletal System and how Bones grow (WEEK 1)
1. The skeletal system consists of bones, cartilage and ligaments forming a strong and flexible framework.
2. Bone development occurs in utero, and during childhood.
3. There are 4 cells involved in bone formation:
- osteoprogenitor cells (stem cells)
- osteoblasts (bone building cells)
- osteocytes (adult osteoblasts)
- osteoclasts (bone chipping away cells)
4. Osseous tissue is a type of connective tissue.
5. Bone can be considered an organ – because it is made up of osseous tissue, cartilage, blood, bone marrow, adipose, nervous and connective tissue. And an organ is defined by the existence of 2 or more tissue types.
6. Bones are classified based on shape not size: they can be long, flat, irregular, or short.
LEVELS OF ORGAINSM
1. The chemical level is the simplest level of organization.
a. Atoms, tiny building blocks of matter, combine to form molecules.
b. Molecules combine in specific ways to form organelles, which are the basic unit of living cells.
2. The cellular level is the smallest unit of life, and varies widely in size and shape according to the cells’ function.
3. The tissue level is groups of cells having a common function.
4. The organ level is made up of discrete structures that are composed of at least two groups of tissues that work together to perform a specific function in the body.
5. The organ system level is a group of organs that work closely together to accomplish a specific purpose.
6. The organismal level is the total of all structures working together to promote life.
Anatomical Position and Directional Terms
1. Anatomical position is a position in which the body is erect, palms face forward, and thumbs point away from the body. Anatomical position is always assumed, regardless of the actual body position and, in anatomical position, right and left refer to the right and left sides of the person viewed.
2. Directional terms are used to explain exactly where one body part is in relation to another.


Regional terms
1. There are two fundamental divisions of the body: the axial region, consisting of the head, neck, and trunk, and the appendicular region, consisting of the appendages—the upper and lower limbs.
2. Regional terms designate specific areas within the axial and appendicular divisions.
Body planes and sections
1. Body planes are flat surfaces that lie at right angles to each other.
a. Sagittal planes are vertical planes that separate the body into right and left parts.
i. A sagittal plane lying directly on the midline of the body is midsagittal, while any sagittal plane off the midline is parasagittal.
b. Frontal planes are vertical planes that separate the body into anterior and posterior parts.
c. Transverse, or horizontal, planes are planes that run horizontally from right to left, and divide the body into superior and inferior parts.
2. Sections are cuts made along or between specific planes, and are used to show different aspects of anatomy.
Body cavities and membranes
Body cavities are spaces within the body that are closed to the outside and protect the internal organs.
A. The dorsal body cavity is the space that houses the central nervous system, and has two subdivisions: the cranial cavity, which houses the brain, and the vertebral cavity, which houses the spinal cord.
B. The ventral body cavity is anterior to and larger than the dorsal cavity and has two main subdivisions: the thoracic cavity and the abdominopelvic cavity.
1. The thoracic cavity is a superior division of the ventral cavity that is subdivided into the pleural cavities that surround each lung, and the medial mediastinum, which includes the pericardial cavity surrounding the heart, and other midline thoracic structures.
2. The abdominopelvic cavity is separated from the thoracic cavity by the diaphragm and consists of two regions: the superior abdominal region contains digestive structures, spleen, and other organs; and the inferior pelvic cavity contains urinary and reproductive structures, and the rectum.
3. Serous membranes within the ventral body cavity are double-layered membranes that cover the inner walls of the ventral cavity and the outer surfaces of organs.
a. Serous membranes within the ventral body cavity are double-layered membranes that cover the inner walls of the ventral cavity and the outer surfaces of organs.
b. The parietal serosa lines the body cavity walls and folds in on itself to form the visceral serosa, which covers the outer surfaces of organs.
c. Serous membranes secrete and are separated by a thin layer of lubrication윤활 fluid called serous fluid, which allows organs to slide without friction along cavity walls and between each other.
d. Serous membranes are named for the specific cavity or organs with which they are associated.
4. The abdominopelvic region is divided into either four quadrants or nine abdominopelvic regions (see pp. 51–52 for a complete list of quadrants and regions).
C. Other Body Cavities
1. There are several smaller body cavities, mostly in the head, and most open to the body exterior (see complete list on p. 50).
The four tissue types

1. EPITHELIAL TISSUE
A. Epithelium occurs in the body as covering or lining epithelium, or as glandular epithelium.
B. Epithelial tissues perform several functions in the body: protection, absorption, filtration, excretion, secretion, and sensory reception.
C. Special Characteristics of Epithelium
1. Polarity: Tissue has an apical surface not attached to surrounding tissues facing either the external environment or the cavity of an internal organ, and a basal surface attached to the underlying connective tissue.
2. Specialized contacts: Adjacent epithelial cells are bound together by specialized contacts such as desmosomes and tight junctions.
3. Supported by connective tissue: A basement membrane, consisting of a basal lamina, and a reticular lamina derived from the collagen of underlying connective tissue.
4. Epithelial tissues are innervated, but avascular receiving nutrients by diffusion from underlying connective tissues.
5. Epithelial tissue has a high regeneration capacity.
D. Classification of Epithelia

1. Each epithelial tissue has a two-part name: the first part indicates the number of layers present, and the second part describes the shape of the cells.
a. Simple epithelia consist of a single layer of cells (as is pseudostratified), while stratified epithelia consist of several layers.
b. Cell shapes may be squamous (flat), cuboidal (box-like), or columnar (column shaped).
2. A simple epithelium consists of a single layer of cells that functions in absorption, secretion, and filtration.
a. Simple squamous epithelium has laterally flattened cells with little cytoplasm, located where filtration or exchange of substances occurs.
b. Simple cuboidal epithelium is characterized by cells that are equally tall and wide, and forms the smallest ducts of glands or kidney tubules.
c. Simple columnar epithelium consists of tall, closely packed cells, and lines the digestive tract.
d. Pseudostratified columnar epithelium contains cells of varying heights that all sit on the basement membrane, giving the appearance of many layers, and secretes or absorbs substances, such as the lining of the respiratory tract.
3. A stratified epithelium is made up of two or more layers of cells that mostly provide protection.
a. Stratified squamous epithelium makes up the external part of the skin, and extends into every body opening.
b. Stratified cuboidal epithelium is found mostly in the ducts of some of the larger glands.
c. Stratified columnar epithelium is found in the pharynx, in the male urethra, and lining some glandular ducts.
d. Transitional epithelium forms the lining of the hollow organs of the urinary system and is specialized to allow cells to change shape and stretch as the organ distends.
E. Glandular Epithelia
1. Endocrine glands are ductless glands that secrete hormones by exocytosis directly into the blood or lymph.
2. Exocrine glands have ducts and secrete their product onto a surface or into body cavities.
a. Unicellular exocrine glands secrete mucus to epithelial linings of the intestinal or respiratory tract.
b. Multicellular exocrine glands consist of a duct, and a group of secretory cells, and may be classified by duct structure, or mechanism of secretion.
i. Simple glands have an unbranched duct, while compound glands have a branched duct.
ii. Secretions in humans may be merocrine, which are products released through exocytosis, or holocrine, which are synthesized products released when the cell ruptures.
*glandular epthelium - mucus (점액)을 내뿜는 조직
*Secretion refers to the production of many substances that the body uses, like sweat, oil, and mucus.
*Excretion only refers to expelling waste from the body.
*innervated - stimulate
*avascular
*merocrine - 부분분비, exocytosis
*holocrine - 완전분비, 세포사멸할때 합성되는 products
2. CONNECTIVE TISSUE

A. Common Characteristics
1. All connective tissue arises from an embryonic tissue called mesenchyme.
2. Connective tissue ranges from avascular to highly vascularized.
3. Connective tissue is composed mainly of nonliving extracellular matrix that separates the cells of the tissue.
B. Structural Components of Connective Tissue
1. Ground substance fills the space between the cells and consists of interstitial fluid, cell adhesion proteins, proteoglycans, and protein fibers.
2. Fibers of the connective tissue provide support.
a. Collagen fibers are extremely strong and provide high tensile strength to the connective tissue.
b. Elastic fibers contain elastin, which allows them to be stretched and to recoil.
c. Reticular fibers are fine, collagenous fibers that form networks where connective tissue contacts other types of tissues.
3. Each major class of connective tissue has a fundamental cell type that exists in immature (-blast) and mature (-cyte) forms.
a. Immature -blast cells are actively mitotic and secrete the fibers and ground substance typical of a specific tissue.
b. Mature-cyte cells are less active, and maintain the health of the tissue, although they may revert to more active
-blast form, if needed for repair.
4. Connective tissues also house other cell types: energy-storing adipose cells, defensive leukocytes, and macrophages, and mast cells, which secrete the anticoagulant heparin, histamine, and proteases and other enzymes.
C. Types of Connective Tissue
-> connective tissue, lymph, bone, cartilage, blood
1. There are two types of connective tissue proper: loose connective tissue, including areolar, adipose, and reticular tissue; and dense connective tissues, consisting of dense regular, dense irregular, and reticular connective tissues.
a. Areolar connective tissue serves to support and bind body parts, contain body fluids, defend against infection, and store nutrients. (loose)
b. Adipose (fat) tissue is a richly vascularized tissue that functions in nutrient storage, protection, and insulation. (loose)
c. Reticular connective tissue forms the internal framework of the lymph nodes, the spleen, and the bone marrow.
(loose, dense)
d. Dense regular connective tissue contains closely packed bundles of collagen fibers running in the same direction and makes up tendons and ligaments. (dense)
e. Dense irregular connective tissue contains thick bundles of collagen fibers arranged in an irregular fashion and is found in the dermis. (dense)
f. Elastic connective tissue is found in select locations and stretches more than dense regular connective tissue.
3. Lymph drains excess amounts of fluid, transports fats and has an important role within the immune system
4. Cartilage grows from chondrocytes, lacks nerve fibers, and is avascular.
a. Hyaline cartilage is the most abundant cartilage, providing firm support with some pliability.
b. Elastic cartilage is found where strength and exceptional stretch are needed, such as the external ear and epiglottis.
c. Fibrocartilage is found where strong support and the ability to withstand heavy pressure are required, such as the intervertebral discs.
5. Bone (osseous tissue) has an exceptional ability to support and protect body structures due to its hardness.
a. Osteoblasts are cells that produce the organic portion of bone matrix, which is then filled in by mineral salts.
b. Osteocytes are cells that are contained in lacunae, small holes that are surrounded by bone matrix.
c. Bone tissue consists of osteons, the structural units of bone tissue, that each have both nerve and blood supply delivered through a central canal.
6. Blood is classified as a connective tissue because it develops from mesenchyme and consists of blood cells and plasma proteins surrounded by blood plasma.
*embryonic - 배아
*avascular - 무혈관
*vascularized - 혈관화
*proteoglycans - 매우 많이 당화된 단백질
*leukocytes - 백혈구
*macrophages- 포식세포, 대식세포
*mast cells - 비만세포, 알레르기 반응의 주요인인 면역세포
*proteases -Proteolysis를 일으키는 효과, Peptide bond가 hydrolysis되는 protein의 분해작용
*mesenchyme - 중간엽
*chondrocyte - 건강한 연골에서 볼 수 있는 세포로 콜라겐 등의 연골기질을 생산하고 유지
3. MUSCLE TISSUE
A. Characteristics
Muscle tissues are highly cellular, well-vascularized tissues responsible for movement, and may be voluntary or involuntary.
B. There are three types of muscular tissue:
1. Skeletal muscle attaches to the skeleton, and is composed of long, cylindrical, multinucleate cells.
2. Cardiac muscle cells are striated, uninucleated, and branched, and are located only in the heart.
3. Smooth muscle cells are unstriated, small, and spindle-shaped, and found in the walls of the hollow organs.
4. NERVOUS TISSUE

Nervous tissue is the main component of the nervous system, which regulates and controls body functions, and is composed of two types of cells:
1. Neurons are specialized cells that have processes that allow them to respond to stimuli (dendrites), and generate and conduct electrical impulses (axons).
2. Supporting cells (neuroglia) are nonconducting cells that support, insulate, and protect the neurons.
CARTILAGE
A. Basic Structure, Types, and Locations
Skeletal cartilages are made from cartilage, surrounded by a layer of dense irregular connective tissue called the perichondrium. There are three types of cartilages:
1. Hyaline cartilage is the most abundant skeletal cartilage and includes the articular, costal, respiratory, and nasal cartilages.
2. Elastic cartilages are more flexible than hyaline and are located only in the external ear and the epiglottis of the larynx.
3. Fibrocartilage is located in areas that must withstand a great deal of pressure or stretch, such as the cartilages of the knee and the intervertebral discs.

B. Growth of Cartilage
1. Appositional growth results in outward expansion due to the production of cartilage matrix on the outer face of the tissue.
2. Interstitial growth results in expansion from within the cartilage matrix due to division of lacunae-bound chondrocytes and secretion of matrix.
BONES
FUNCTIONS OF BONE:
1. Support: bones provide a framework for the body, and surrounds soft organs.
2. Protection: bones protect the brain and vital organs.
3. Anchorage: skeletal muscles attach to bones with tendons.
4. Mineral storage: bones store calcium and phosphate.
5. Blood cell formation: hematopoieis occurs within red bone marrow.
6. Triglyceride storage: fat is stored in yellow bone marrow.
7. Hormone production: production of osteocalcin, that helps regulate insulin secretion.
CLASSIFICATION OF BONES (OF THE SKELETON):
A. There are two main divisions of the bones of the skeleton: the axial skeleton, and the appendicular skeleton.
1. The axial skeleton consists of the skull, vertebral column, and rib cage, that protect, support, or carry other body parts.
2. The appendicular skeleton consists of the bones of the upper and lower limbs, and the girdles that attach them to the axial skeleton, which serve to move the body from place to place and manipulate our environment.
B. Bones are classified by their shape.
1. Long bones are longer than they are wide, have a definite shaft축 and two ends, and consist of all limb bones except patellast슬개골 and wrist and ankle bones.
2. Short bones are somewhat cube-shaped and include the carpals, tarsals, and patellas.
3. Flat bones are thin, flattened, often curved bones that include most skull bones, the sternum, scapulae, and ribs.
4. Irregular bones have complicated shapes that do not fit in any other class, such as the vertebrae and hip bones.
ANATOMY OF BONE
A. Gross Anatomy
1. Compact and Spongy Bone
a. All bone has a dense outer layer consisting of compact bone that appears smooth and solid.
b. Internal to compact bone is spongy bone, which consists of needle-like or flat pieces, called trabeculae.

2. Structure of Short, Irregular, and Flat Bones
a. Short, irregular, and flat bones consist of thin plates of periosteum-covered compact bone on the outside and endosteum-covered spongy bone inside, called diploë, which houses bone marrow between the trabeculae.
3. Structure of a Typical Long Bone
a. Long bones have a tubular diaphysis, consisting of a bone collar surrounding a hollow medullary cavity, which is filled with yellow bone marrow in adults.
b. Epiphyses are at the ends of the bone, and consist of internal spongy bone covered by an outer layer of compact bone, and a thin layer of articular cartilage.
c. The epiphyseal line is located between the epiphyses and diaphysis and is a remnant of the epiphyseal plate, the hyaline cartilage that provides lengthwise growth of bone.
d. The external surface of the bone is covered by the periosteum, the location of osteogenic cells.
e. The internal surface of the bone is lined by a connective tissue membrane called the endosteum, a location of osteogenic cells within the bone.
f. A nutrient artery and vein, as well as nerves, serve the bone marrow and spongy bone through an opening, the nutrient foramen, in the diaphysis, and then branch outward to supply the compact bone.
g. Epiphyses have blood and nerve supply similar in arrangement to those serving the diaphysis.

4. Hematopoietic Tissue in Bones
a. Red bone marrow is located within the trabecular cavities of the spongy bone in long bones and in the diploë of flat bones.
b. In long bones, red bone marrow is found in all medullary cavities and all areas of spongy bone of infants, but in adults, distribution is restricted to the proximal epiphyses of the humerus and femur.
because infants need a massive amount of blood cells to produce blood as their immune system isn't mature enough.
As they get older, part of their red bone marrow changes into yellow bone marrow for energy storage, and also their immune system is mature enough so their red blood marrow is reduced
5. There are three categories of bone markings:
a. Projections that function as attachment sites for tendons and ligaments.
b. Surfaces that form joints.
c. Depressions and openings for the passage of blood vessels and nerves.
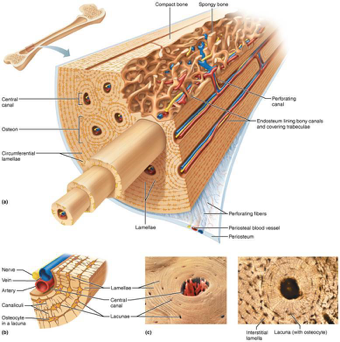
B. Microscopic Anatomy of Bone
1. Bone tissue contains five types of cells: bone stem cells, called osteoprogenitor cells, osteoblasts that secrete bone matrix, osteocytes and bone lining cells that monitor and maintain bone matrix, and osteoclasts that are involved in bone resorption.
2. The structural unit of compact bone is the osteon, or Haversian system, a series of concentric tubes of bone matrix, called lamellae
a. The central canal runs through the center of each osteon, and allows passage of blood vessels and nerves.
b. Perforating, or Volkmann’s, canals lie at right angles to the long axis of the bone, and connect the blood and nerve supply of the periosteum to that of the central canals and medullary cavity.
c. Lacunae, small holes housing the osteocytes, are found at the junctions of the lamellae and are connected to each other and the central canal via a series of hair-like channels, canaliculi.
d. Lamellae located just beneath the periosteum and extending around the entire circumference of the bone are called circumferential lamellae, while interstitial lamellae lie between intact osteons, filling the spaces in between.
CHEMICAL COMPOSITION OF BONE
1. Organic components of bone include cells and osteoid (ground substance and collagen fibers), which contribute to the flexibility and tensile strength of bone.
2. Inorganic components make up 65% of bone by mass, and consist of hydroxyapatites, mineral salts (largely calcium phosphates), that account for the hardness and compression resistance of bone
OSSIFICATION OF BONE
A. Prenatal Bone Growth (태아기)
1. In endochondral ossification, bone tissue replaces hyaline cartilage, forming all bones below the skull except for the clavicles.
a. Initially, osteoblasts secrete osteoid, creating a bone collar around the diaphysis of the hyaline cartilage model.
b. Cartilage in the center of the diaphysis calcifies and deteriorates, forming cavities.
c. The periosteal bud invades the internal cavities and spongy bone forms around the remaining fragments of hyaline cartilage.
d. The diaphysis elongates as the cartilage in the epiphyses continues to lengthen, and a medullary cavity forms through the action of osteoclasts within the center of the diaphysis.
e. The epiphyses ossify shortly after birth through the development of secondary ossification centers.
2. Intramembranous ossification forms membrane bone from fibrous connective tissue membranes, and results in the cranial bones and clavicles.
a. Mesenchymal cells differentiate into osteoblasts, and form an ossification center.
b. Osteoblasts secrete osteoid, that calcifies, trapping osteoblasts, which become osteocytes.
c. Immature spongy bone and the periosteum form as osteoid is deposited between embryonic vessels.
d. Trabeculae just beneath the periosteum are remodeled into compact bone, while red bone marrow develops and fills the spaces between maturing spongy bone.
B. Postnatal Bone Growth (산후)
1. Events at four distinct zones within a long bone contribute to growth in length:
a. At the proliferation zone, cells facing the epiphysis rapidly divide, increasing length of the bone.
b. At the hypertrophic zone, older chondrocytes near the diaphysis enlarge, resulting in erosion and enlargement of the lacunae.
c. At the calcification zone, chondrocytes die, allowing the invasion of blood vessels, and the surrounding matrix calcifies.
d. At the ossification zone, the calcified spicules are broken down by osteoclasts, allowing osteoblasts to fill in the area with new spongy bone.
2. Growth in width, or thickness, occurs through appositional growth due to deposition of bone matrix by osteoblasts beneath the periosteum
3. Hormonal Regulation of Bone Growth
a. During infancy and childhood, the most important stimulus of epiphyseal plate activity is growth hormone from the anterior pituitary, whose effects are modulated by thyroid hormone.
b. At puberty, testosterone and estrogen promote a growth spurt, ultimately resulting in the closure of the epiphyseal plate.
1. In adult skeletons, bone deposit and resorption occur beneath the periosteum(골막) and endosteum.
2. Osteoclasts secrete acid and lysosomal enzymes that break down bone matrix, absorb the components, and release them to the interstitial fluid.
BONE DEPOSITION
1. An osteoid seam of gauzy-looking bone indicates the area of new bone deposition; it is separated from older mineralized bone by a transition zone called a calcification front.
2. Osteoid becomes calcified through stimulation of osteoblasts, causing the release matrix vesicles containing alkaline phosphatase, that combine free Ca++ and phosphates, forming crystals that give rise to hydroxyapatite.
BONE REMODELLING
1. Bone remodeling serves two purposes: ensures Ca++ homeostasis, and maintains strength of bone tissue.
2. Hormonal control of remodeling is mostly used to maintain blood calcium homeostasis and balances activity of parathyroid hormone and calcitonin.
a. Parathyroid hormone (PTH) stimulate osteoclasts to resorb bone, releasing Ca++ to the blood, while calcitriol increases Ca++ absorption in the intestines.
3. Wolff’s law states that bone grows or remodels in ways that allow it to withstand the stresses it experiences, due to factors such as mechanical stress and gravity.
A. Fractures are breaks in bones and are classified by the position of the bone ends after fracture, completeness of break, and whether the bone ends penetrate the skin.
B. Repair of fractures involves four major stages:
1. Hematoma formation: torn vessels result in bleeding that soon forms a clot.
2. Fibrocartilaginous callus forms: fibroblasts and chondroblasts invade the fracture site and secrete a cartilaginous matrix that calcifies.
3. Bony callus forms: within the fibrocartilaginous callus, osteoblasts begin forming spongy bone.
4. Bone remodeling occurs: for several months, the bony callus is remodeled, so that excess material on the diaphysis and in the medullary cavity is removed.
A. Osteomalacia and Rickets
1. Osteomalacia includes a number of disorders in adults in which the bone is inadequately mineralized.
2. Rickets is inadequate mineralization of bones in children caused by insufficient calcium in the diet or by a vitamin D deficiency.
B. Osteoporosis refers to a group of disorders in which the rate of bone resorption exceeds the rate of formation.
1. Bones have normal bone matrix, but bone mass is reduced and the bones become more porous and lighter, increasing the likelihood of fractures.
2. Older women are especially vulnerable to osteoporosis, due to the decline in estrogen after menopause.
3. Other factors that contribute to osteoporosis include insufficient exercise or immobility, a diet poor in calcium, vitamin D, or protein, smoking, certain hormone-related conditions, or alcohol and certain drugs.
C. Paget’s disease is characterized by excessive, random bone deposition and resorption, with the resulting bone abnormally high in spongy bone. It is a localized condition that results in deformation of the affected bone.
SKELETAL BONE DEVELOPMENT
A. The skeleton derives from embryonic mesenchymal cells, with ossification occurring at precise times: Most long bones have obvious primary ossification centers by 12 weeks, of gestation.
B. At birth, most bones are well ossified: After birth, bones form secondary ossification centers, but epiphyseal plates remain throughout childhood, as the site of longitudinal bone growth.
C. Throughout childhood, bone growth exceeds bone resorption; in young adults, these processes are in balance; in old age, resorption exceeds formation.
Topic 1.2 The Axial Skeleton (WEEK 1)
The skeletal system includes all of the bones, cartilages, and ligaments of the body that support and give shape to the body and body structures, whereas the skeleton consists of the bones of the body. For adults, there are 206 named bones in the skeleton. Younger individuals have higher numbers of bones because some bones fuse together during childhood and adolescence. The primary functions of the skeleton are to provide a rigid, internal structure that protects internal organs and supports the weight of the body, and to provide a structure upon which muscles can act to produce movements of the body. The bones of the skeleton also serve as the primary storage site for important minerals such as calcium and phosphate. The bone marrow found within bones stores fat and houses the blood-cell producing tissue of the body.
The skeleton is subdivided into two major divisions—the axial and appendicular.
THE AXIAL SKELETON
The axial skeleton forms the vertical, central axis of the body and includes all bones of the head, neck, chest, and back (Figure 7.1.1). It serves to protect the brain, spinal cord, heart, and lungs. It also serves as the attachment site for muscles that move the head, neck, and back, and for muscles that act across the shoulder and hip joints to move their corresponding limbs.
The axial skeleton of the adult consists of 80 bones, comprising the skull, the vertebral column, and the thoracic cage. The skull is formed by 22 bones. Also associated with the head are an additional seven bones, including the hyoid bone (found in the upper neck) and the ear ossicles (three small bones found in each middle ear). The vertebral column consists of 24 bones, each called a vertebra, plus the fused vertebrae of the sacrum and coccyx. The thoracic cage includes 12 pairs of ribs, and the sternum, the flattened bone of the anterior chest.

This diagram shows the human skeleton and identifies the major bones. The left panel shows the anterior view (from the front) and the right panel shows the posterior view (from the back).
– Axial and Appendicular Skeleton:
The axial skeleton supports the head, neck, back, and chest and thus forms the vertical axis of the body. It consists of the skull, vertebral column (including the sacrum and coccyx), and the thoracic cage, formed by the ribs and sternum. The appendicular skeleton is made up of all bones of the upper and lower limbs and the girdles which attach them to the axial skeleton.
The Skull
A. The cranial and facial bones form the framework of the face, and contain cavities for special sense organs, provide openings for air and food passage, secure the teeth, and anchor muscles of facial expression.
B. Except for the mandible, which is joined to the skull by a movable joint, most skull bones are flat bones joined by interlocking joints called sutures
C. Overview of Skull Geography
1. The cranium is divided into a vault, forming the superior, lateral, and posterior aspects, and a base, forming the inferior aspect.
2. The anterior aspect of the skull is formed by facial bones, and the remainder is formed by a cranium, which is divided into the cranial vault, or calvaria, and cranial base.
3. The cavities of the skull include the cranial cavity, which houses the brain, along with ear cavities, nasal cavity, and orbits, which house the eyeballs.
4. The skull has about 85 named openings that provide passageways for the spinal cord, major blood vessels serving the brain, and the cranial nerves.
D. Cranial Bones
The cranium consists of eight strong, superiorly curved bones.
E. Facial Bones
The facial skeleton is made up of 14 bones, of which only the mandible and vomer are unpaired.
F. The hyoid bone lies inferior to the mandible in the anterior neck. It is the only bone that does not articulate directly with any other bone.
G. Special Characteristics of the Orbits and Nasal Cavity
1. The orbits are bony cavities that contain the eyes, muscles that move the eyes, and tear-producing glands.
2. The nasal cavity is constructed of bone and hyaline cartilage, covered by a mucous membrane that serves to warm and moistened inhaled air, and trap debris.
3. Paranasal sinuses, located within the frontal, sphenoid, ethmoid, and maxillary bones, are air-filled spaces, lined with a mucous membrane, that are clustered around the nasal cavity that lighten the skull and enhance resonance of the voice.
The vertebral column
General Characteristics
1. The vertebral column consists of 26 irregular bones, forming a flexible, curved structure extending from the skull to the pelvis that surrounds and protects the spinal cord and provides attachment for ribs and muscles of the neck and back.
Divisions and Curvatures
a. The vertebrae of the spine fall in five major divisions: seven cervical, twelve thoracic, five lumbar, five fused vertebrae of the sacrum, and four fused vertebrae of the coccyx.
b. The curvatures of the spine increase resiliency and flexibility of the spine.
c. The cervical and lumbar curvatures are concave posteriorly, and the thoracic and sacral curvatures are convex posteriorly.
3. The major supporting ligaments of the spine are the anterior and posterior longitudinal ligaments, which run as continuous bands down the front and back surfaces of the spine, supporting the spine and preventing hyperflexion and hyperextension.
4. Intervertebral discs are cushion-like pads that act as shock absorbers and allow the spine to flex, extend, and bend laterally.
The thoracic cage
The thoracic cage consists of the thoracic vertebrae dorsally, the ribs laterally, and the sternum and costal cartilages anteriorly, forming a protective cage around the organs of the thoracic cavity, and providing support for the shoulder girdles and upper limbs.
General Skeleton Basic Tutorial - Anatomy Tutorial
General Skeleton - 3D Models, Video Tutorials & Notes | AnatomyZone
3D video anatomy tutorial covering the basics of the bones of the skeleton.
anatomyzone.com
https://aclandanatomy.com/index.aspx
Home | Acland's Video Atlas of Human Anatomy
Real Movement. Exquisite Dissections. Acland's Video Atlas of Human Anatomy contains nearly 330 videos of real human anatomic specimens in their natural colors, including 5 new, groundbreaking videos of the inner ear. Dr. Robert Acland presents moving stru
aclandanatomy.com
Skull - 3D Models, Video Tutorials & Notes | AnatomyZone
We use cookies on our website to give you the most relevant experience by remembering your preferences and repeat visits. By clicking “Accept”, you consent to the use of ALL the cookies.
anatomyzone.com
How can physical activities strengthen bone density?
-> osteocytes can sense the pressure/workload on the bone and respond to triggering osteoblasts to increase bone density
+
conversely when bone experiences reduce loading conditions (such as long-term bedrest)
remodeling increases
'Griffith college Tri3 2022 > 1016MSC (AnP)' 카테고리의 다른 글
| WEEK3 - Muscular system (1) learning contents (0) | 2022.11.04 |
|---|---|
| WEEK3 - Muscular system (1) resources + note (0) | 2022.11.04 |
| WEEK2 - Skeletal system (2) learning contents (0) | 2022.11.02 |
| WEEK1 - Skeletal system (1) resources + notes (0) | 2022.10.29 |
| WEEK0 - Intro (0) | 2022.10.22 |


