Learning objectives
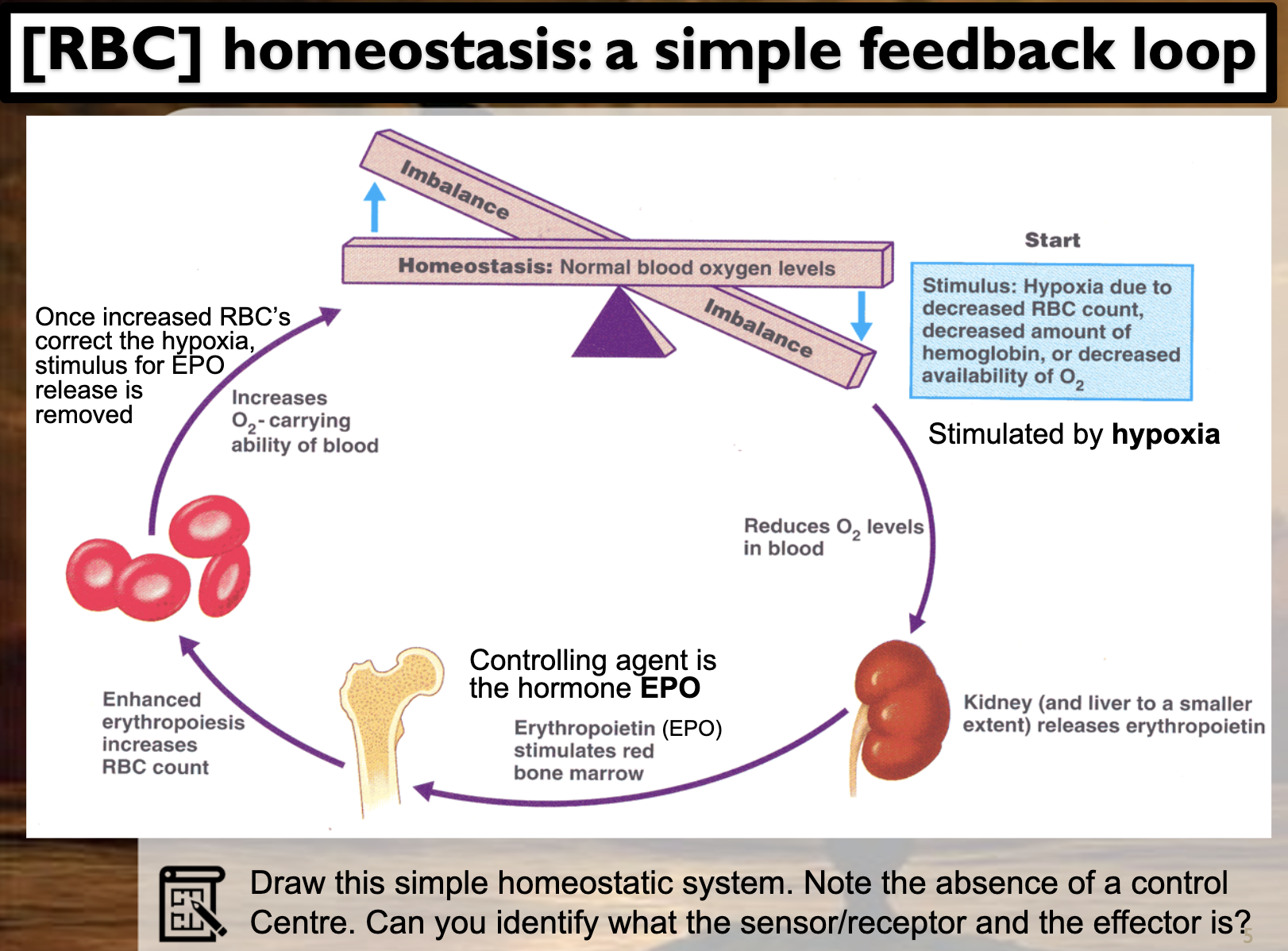
-Understand the primary stimulus for release of erythropoietin (EPO), and how this affects red blood cell production.
-RBC homeostasis: Describe the related negative feedback loop in terms of it’s complexity, and how rising RBC concentrations are countered.
EPO, RBC, negative feedback loop, no control center
Kidney detects the hypoxia, which refers to the low oxygen level in the blood. It is a stimulus for erythropoietin being released from the kidney, which then stimulates red bone marrow in the bone to produce red blood cell (erythrocyte). This process is called erythrogenesis. Erythrogenesis increases RBC concentration in the blood and it increases the oxygen level in the blood also. It removes the stimulus to the kidney to secrete erythropoietin(EPO). It is negated with negative feedback loop.
-Describe how treatment with large amounts of EPO can cause death in athletes who undertake prolonged, high intensity aerobic function, and why athletes might be directed to train at high altitude or to sleep in low-oxygen tents.
ATHLETES, EPO
Large amounts of EPO increase the viscocity of the blood, which blocks the circulation of the blood. It can cause heart attack, stroke, and cardiovascular diseases.
Athletes are directed to train at high altitude or to sleep in low-oxygen tents. It makes their body to increase the set point of the RBC, which in turns make them possess more RBC. As their body produce more RBC and the concentration of haemoglobin in the blood increases, transporting oxygen to the muscles becomes much easier which means they can operate more effectively. They can perform better.
-Draw the homeostatic flow diagram, the hormones involved and tissues involved when blood concentrations of calcium either rise or fall, nothing where the primary stimulus is monitored in each case
Ca2+ regulation
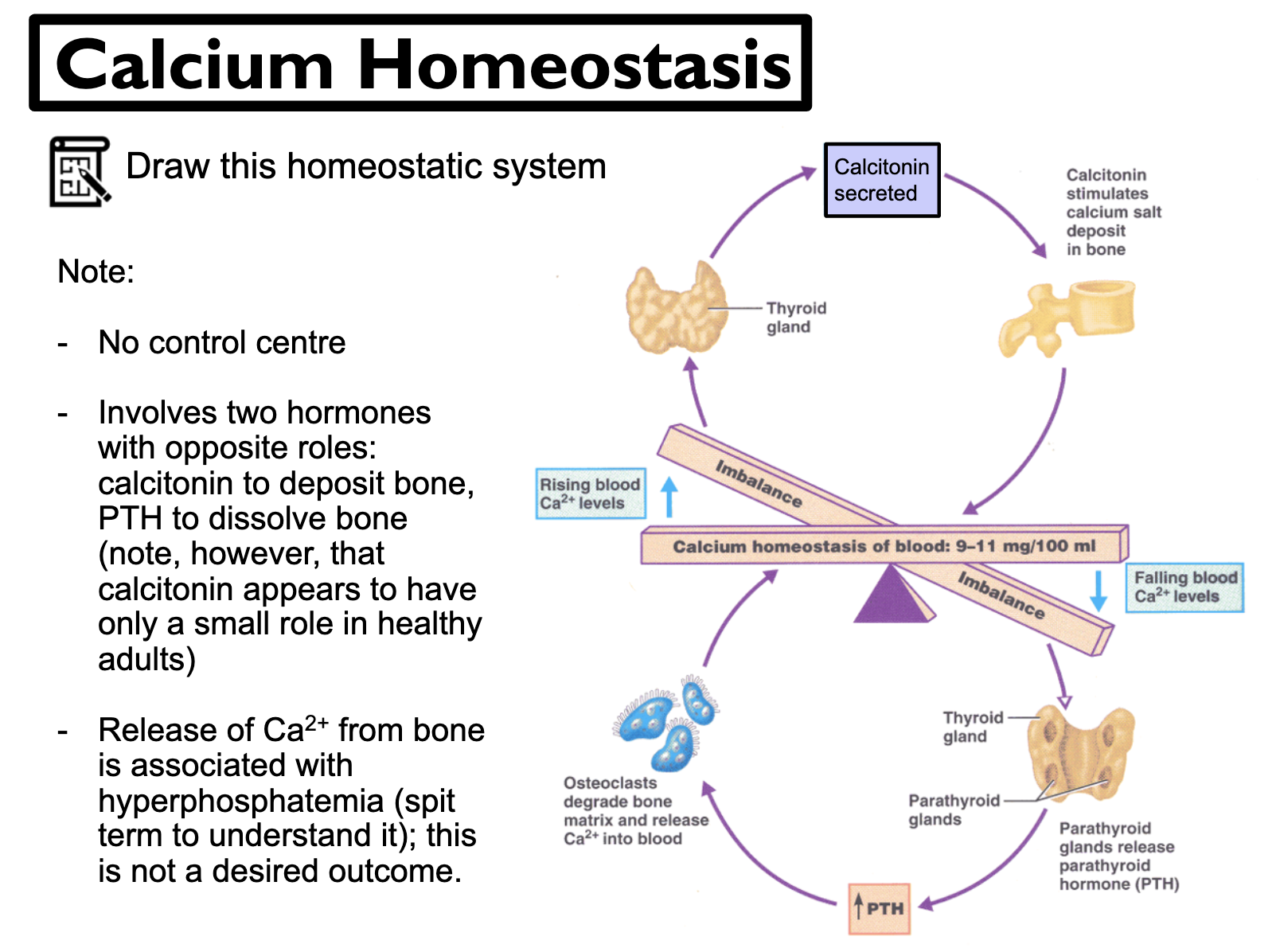
When the Calcium concentration in blood falls, cells in the parathyroid gland detect it as a stimulus and secrete parathyroid hormone. It then activates osteoclasts to break down the bone to release Ca2+ into the blood. It also increases Ca2+ reabsorption in the kidney, and stimulates kidney to activate vitamin D, which increases Ca2+ absorption in the intestine. When the Ca2+ increases, the stimulus is negated.
When the Calcium concentration in blood rises, calcitonin is released from the thyroid gland. It is an antagonist to the PTH. Calcitonin supresses osteoclasts activity and it stimulate kidney to excrete more Ca2+ in the urine.
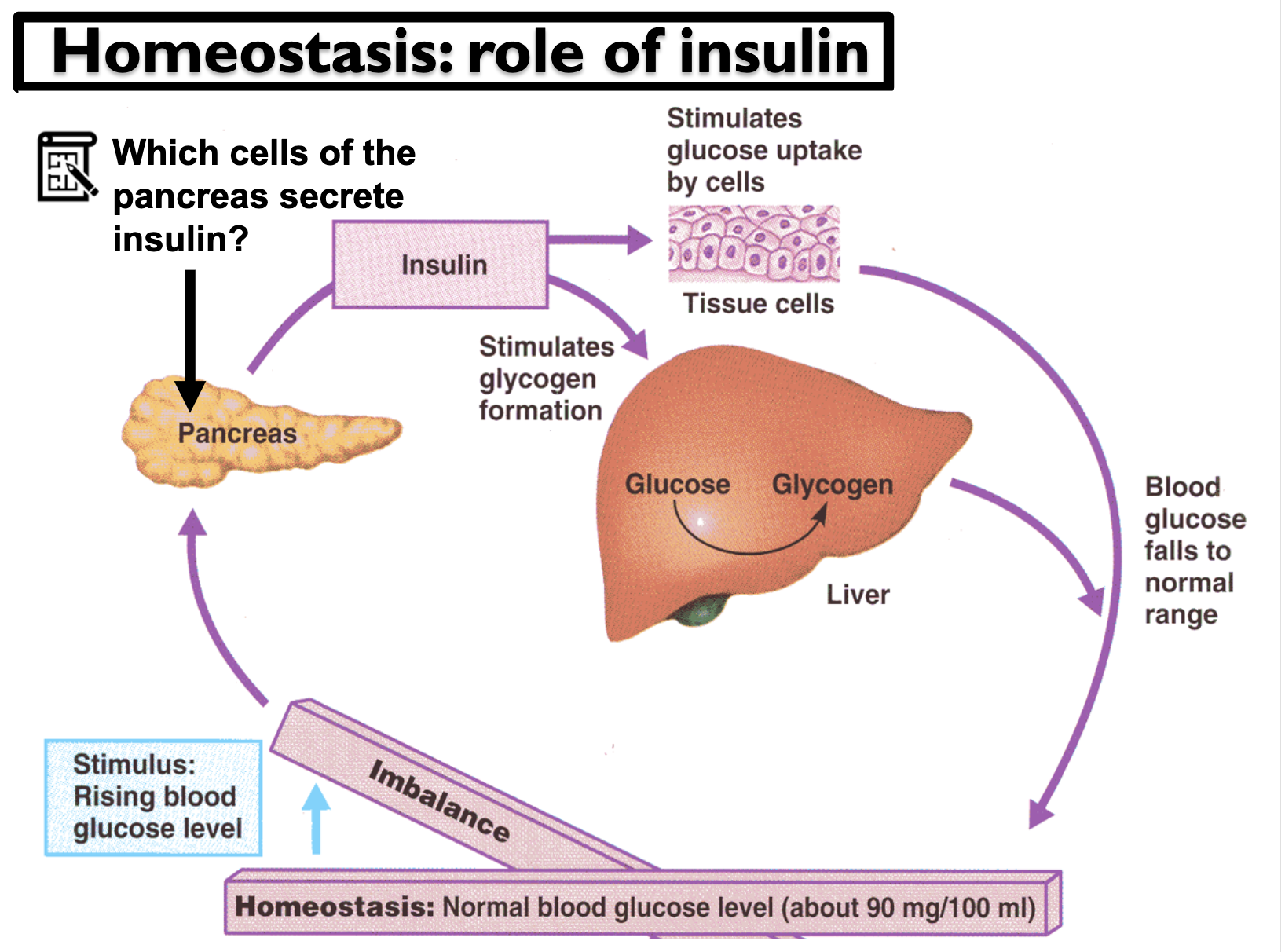
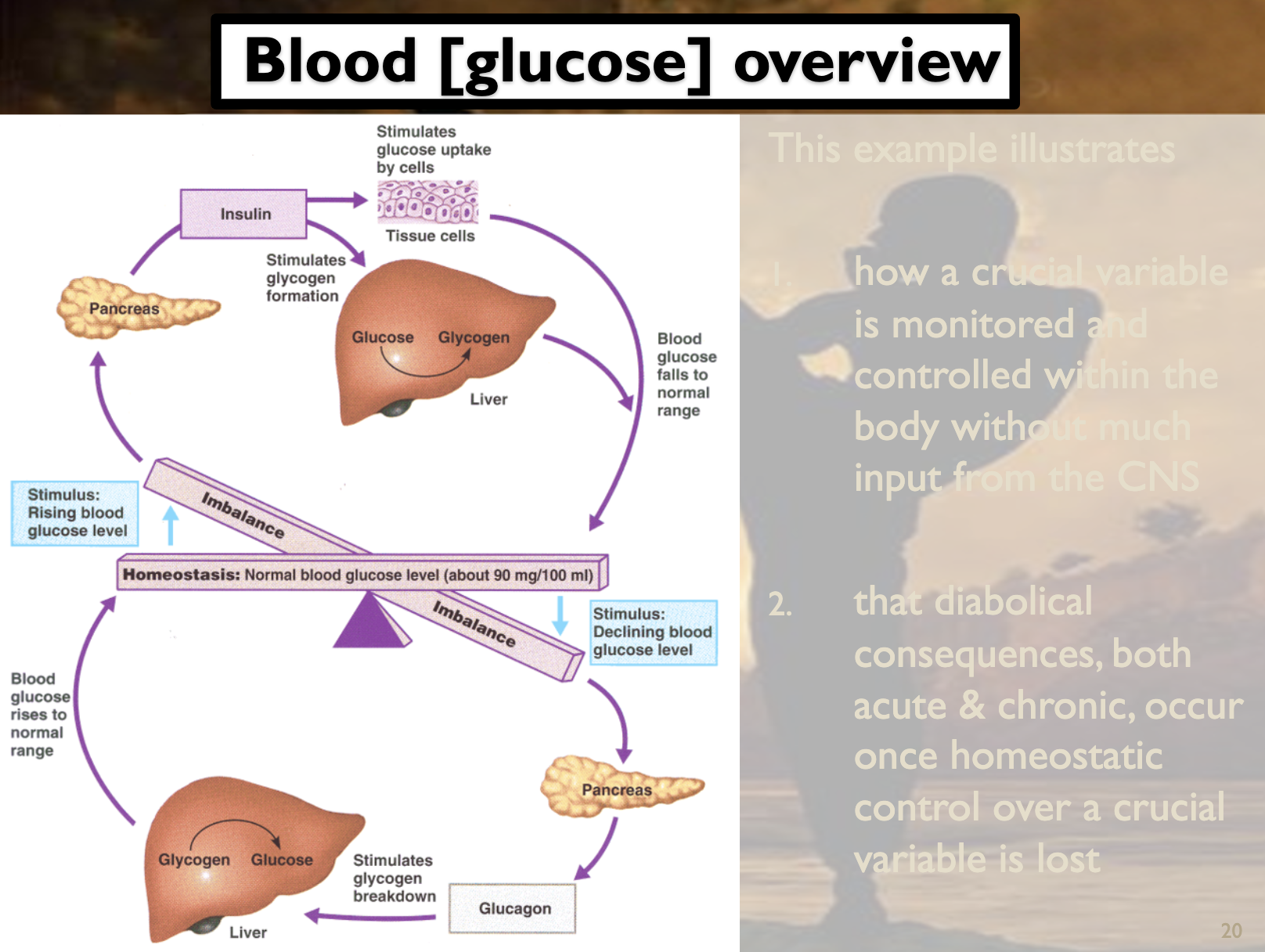
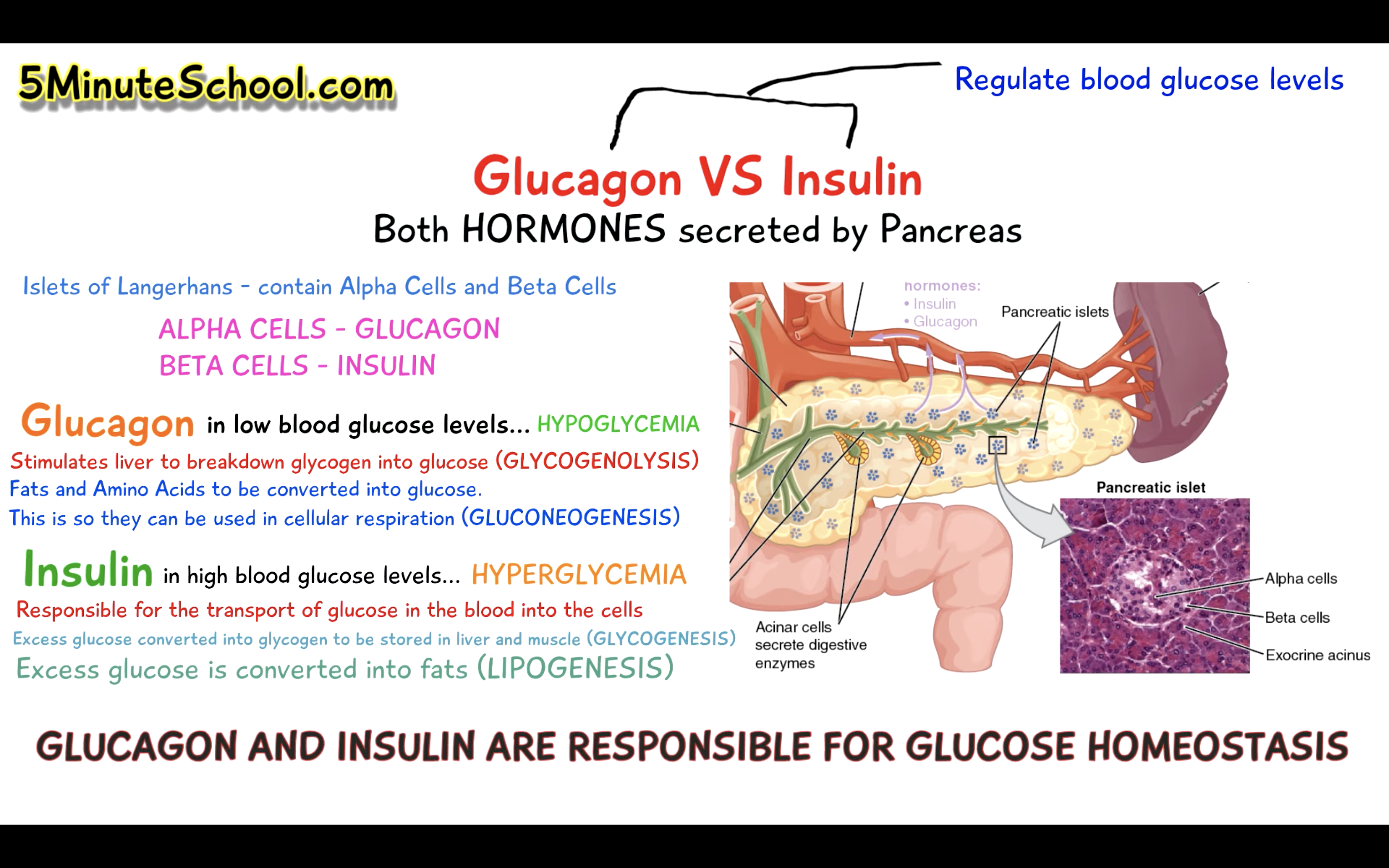
-Be able to describe the role of insulin in homeostasis of blood glucose levels; what stimulates production, where does insulin originate, and what happens as a result of its secretion?
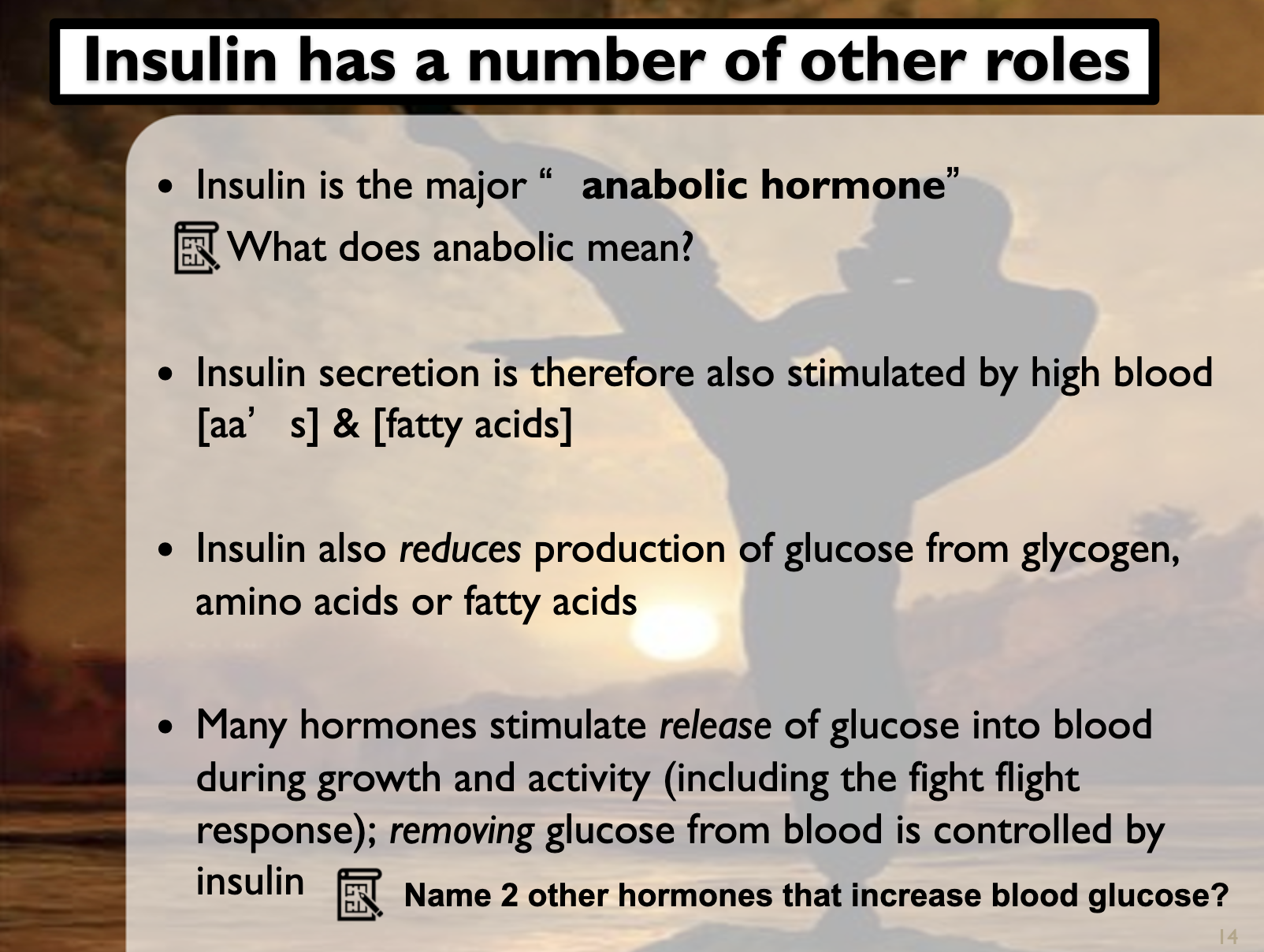
INSULIN
Insulin is produced in the beta cells of the pancreas. It decreases the blood glucose level by producing glycogen from the glucose in the liver. It is stimulated by the high glucose level in the blood stream but it can also secreted by high aminoacids and lipids concentration. It inhibits aminoacids and lipids from becoming glucose, and increases protein synthesis and fat storage. As a result, blood glucose level decreases.
Insulin is a water soluble hormone, which binds to the receptors in the cell membrane. The receptors stimulates G protein which brings about the conversion of ATP to cAMP by an enzyme. cAMP starts the cascade which results in GLUT4 transporter doing exocytosis to the cell membrane. The Facilitated diffusion of the glucose occurs via the GLUT4 transporter, which means glucose flows down the concentration gradient to the body. This process increases the glucose uptake in the cell.
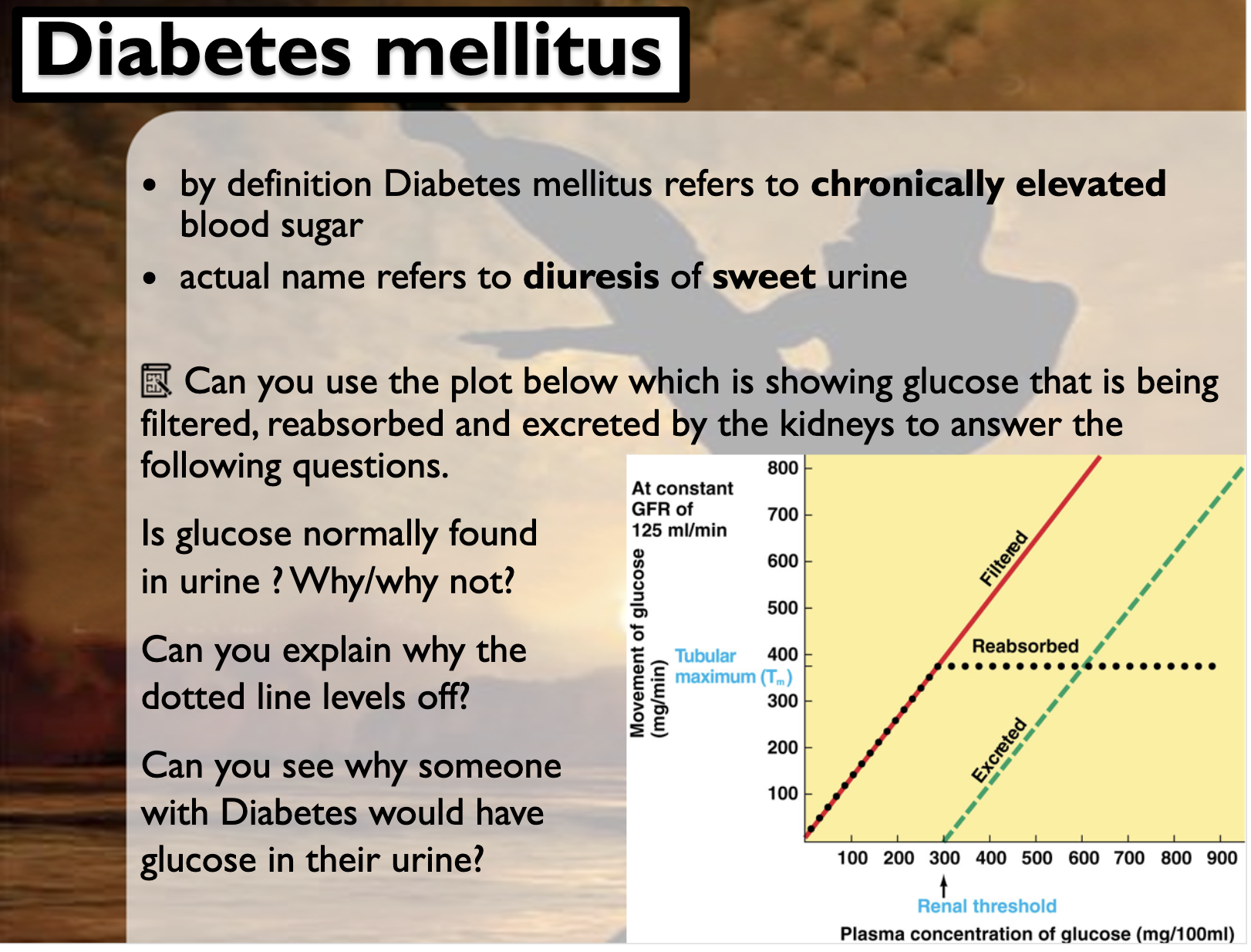
-Be able to analyse a graph describing the relationship between [glucose] in primary filtrate vs re-uptake from the primary filtrate, incorporating the concepts of Tmax and carrier saturation.
The red line is the Primary filtrate, which shows that the more we retain glucose in our body, the more movement of the glucose occurs.
(primary filterate is from glomerular capsule, and the plasma and the filterate concentrations of glucose and NaCl are essentially identical. Primary filterate contains glucose, amion acids, water, and waste products such as urea.)
Our body has the renal threshold and tubular maximum to reabsorb certain amount of the glucose and excrete the rest of them.
Glucose is reuptaken by the secondary active transport, Na+ glucose transporter.
When the transporters are all packed (carrier saturaton), excess glucose is excreted by the urine
(when the carriers are all saturated, it reaches to the Tubular maximum. Tm refers to the maxmium amount of substances which can be reabsorbed to the body. The excess of the substances are excreted by the urine).
The renal threshold shows the maximum amount of glucose that can be reabsorbed. Over the renal threshold, {Primary filtrate - (re-uptake from the primary filterate)} shows the amount of excreted of glucose.

-Define diabetes mellitus and be able to distinguish between the 2 types. Understand reasons for the common renal symptoms of increased water loss and presence of glucose in urine, and describe some of the long term consequences if the condition is left chronically untreated.
DIEBETES MELLITUS
Diebetes mellitus type1 and 2 both accompany high glucose level in blood chronically.
DM Type 1 is caused by damaged beta-cells in the pancreas by the auto immune system's attack. As beta-cells are destroyed, they cannot produce insulin at all. DM Type 2 is caused by increased insulin resistance due to poor diet and lack of exercise. Unlike to Type1 diebetes, type 2 can be improved by doing exercise and having balanced diet.
-Increased water loss -> high glucose level in blood makes more glucose to be secreted by the kidney. When excess glucose is excreted into the urine, it drags along fluids/water.
-Sweet urine -> As glucose transporter in the nephron is saturated, rest of the glucose is secreted by the urine.
-Long term consequences if the condition is left chronically untreated ->
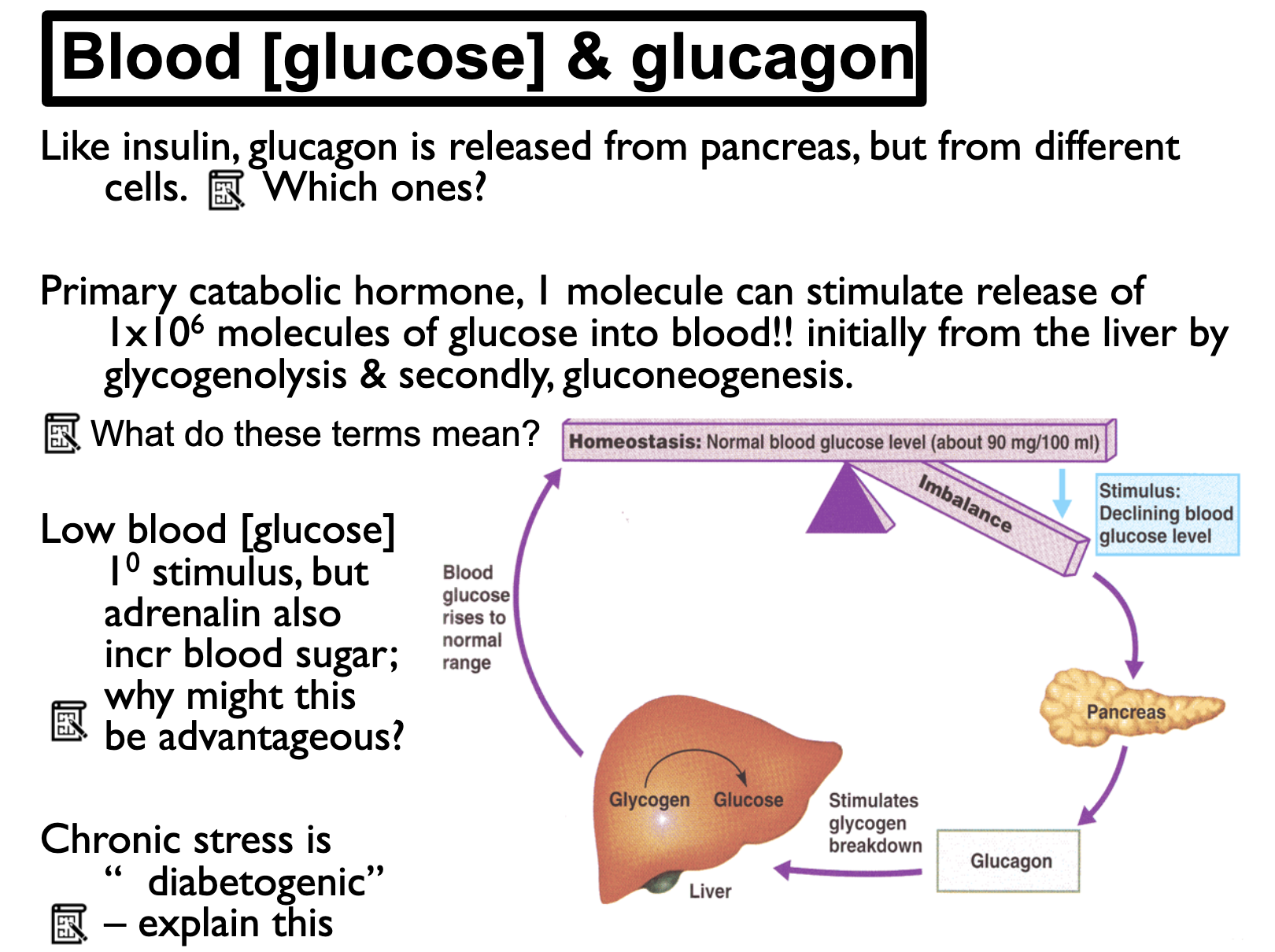
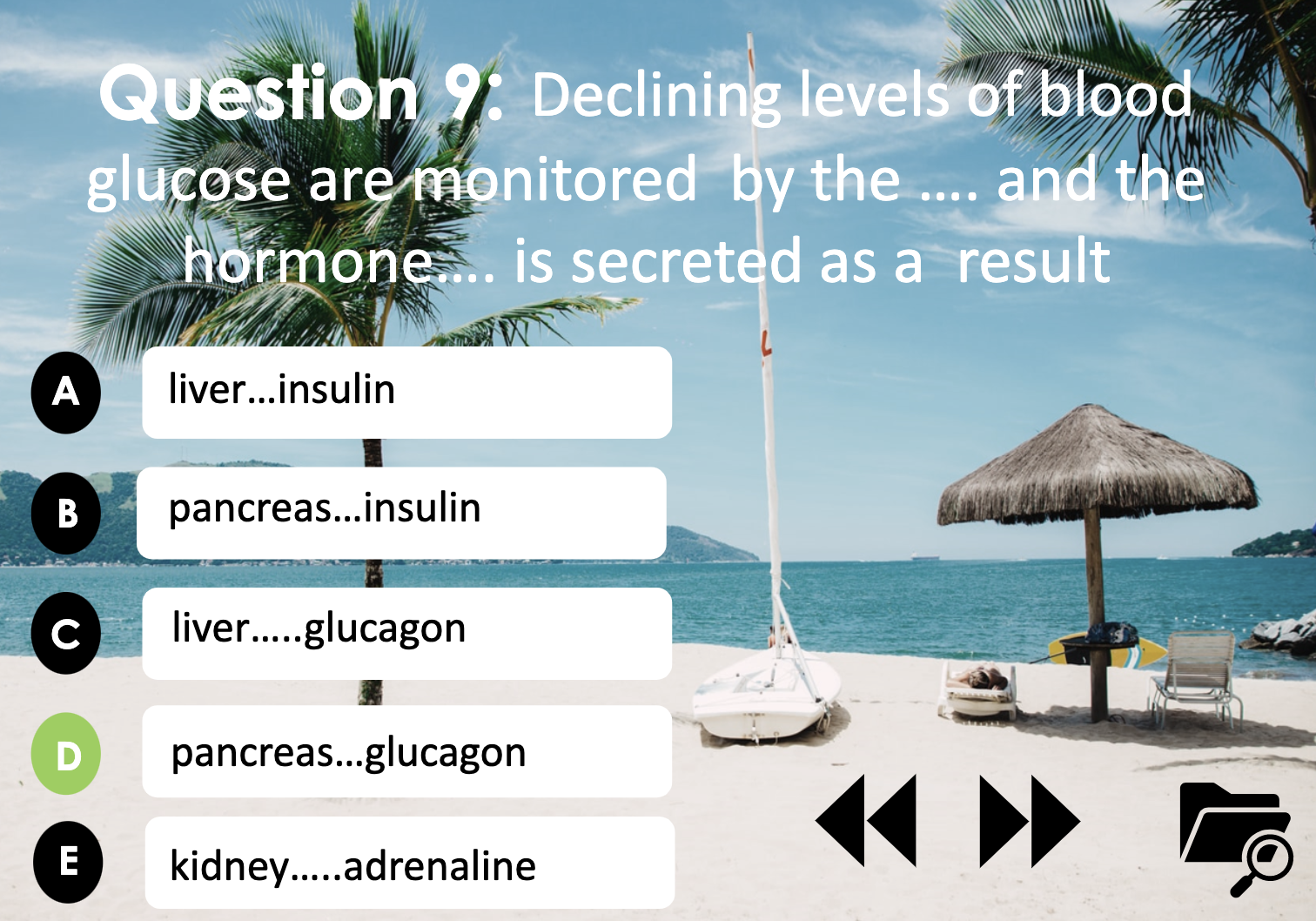
-Glucagon: what stimulates its release, what does in achieve, why it is termed a primary catabolic agent, and, by splitting the terms, explain how glucagon stimulates both gluconeogenesis and glycogenolysis.
GLUCAGON
Low glucose level stimulates the glucagon to be released from the alpha-cell in the pancreas. It breaks down the glycogen(bigger molecule) stored in the liver into glucose(smaller molecule). Catabolic agents break down bigger molecules into smaller molecules and release energy. Glucagon is responsible for glycogenolysis and gluconeogenesis.
Gluconeogenesis is splitted into gluco/ neo/ genesis. Glucose (gluco) can be newly (neo) made (genesis) with the source of lipids and aminoacids, which is the process of synthesis. (synthesis)
Glycogenolysis can be splitted into glycogen/ lysis. It means that glucose can be produced by breaking down (lysis) the Glycogen (glycogen).
-Why might chronic stress be diabetogenic?
STRESS and DIABETOGENIC
Stress is a stimulus for cortisol secretion. Cortisol increases the blood glucose level to cope with stressful situations. Increased glucose level allows glucose molecules to travel all other body parts so that they can be used as an energy source to deal with that stress. As diabetogenic refers to a persistent elevation in blood-glucose, chronic stress can be a diabetogenic agent by the cortisol activity.
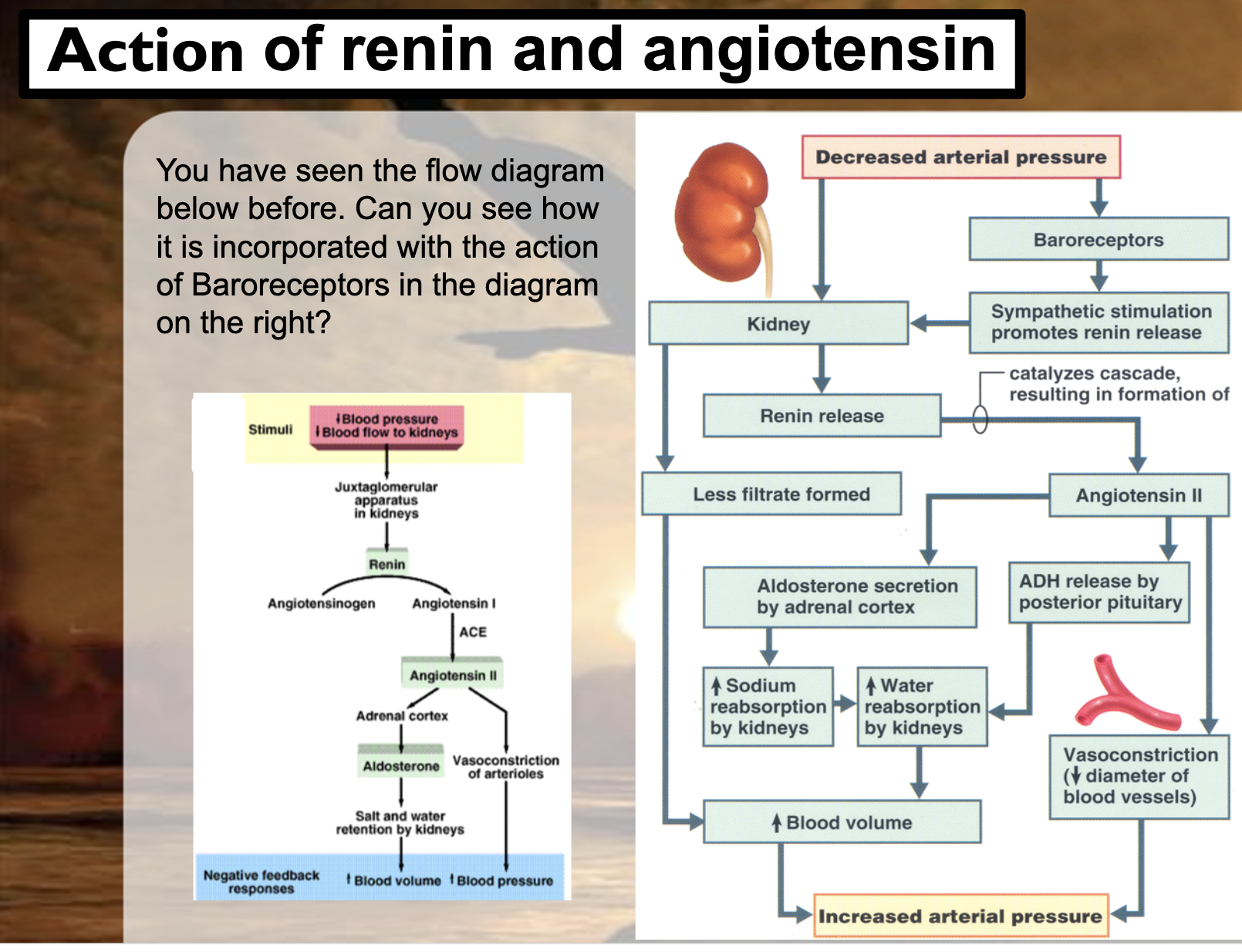
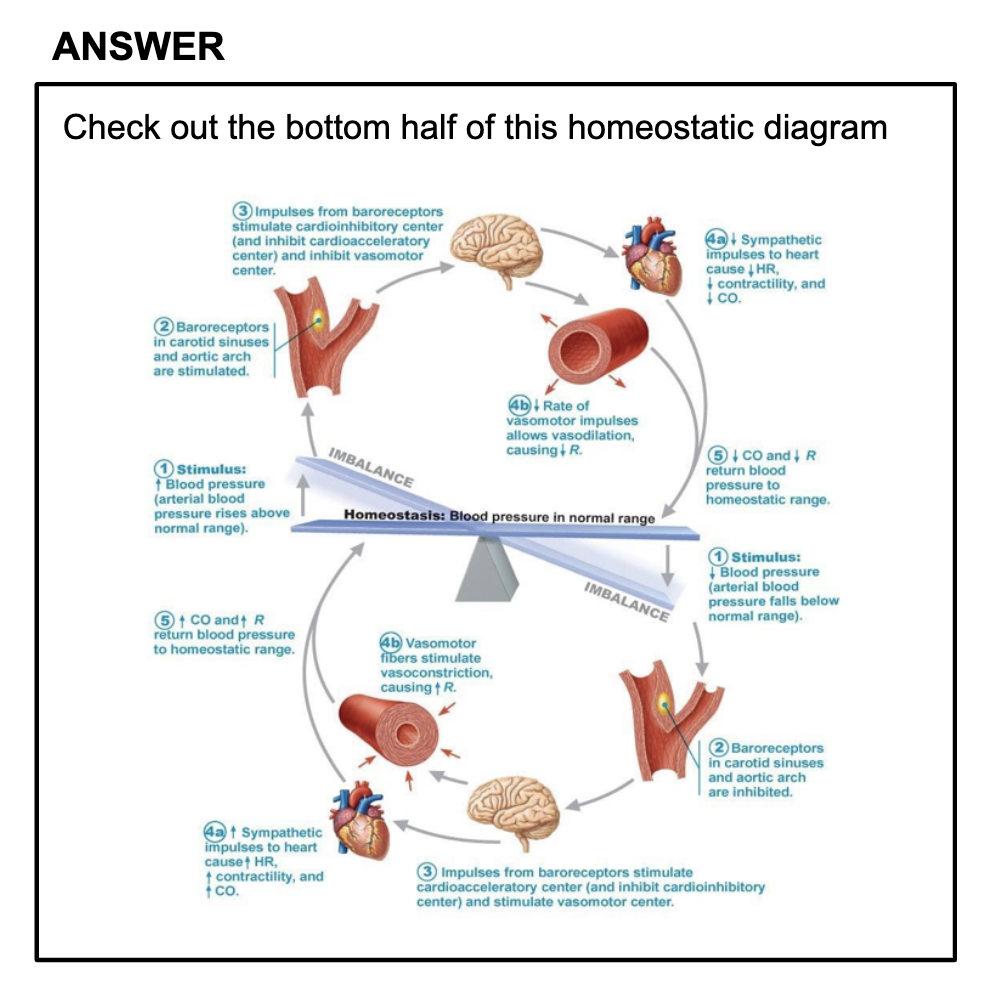
-Understand the role of baroreceptors in the homeostasis of BP.
Baroreceptors are sensory neurons usually located in the blood vessels toward the brain and the heart. They are known as strectch receptors as they sense the stretch as a stimulus. When the blood pressure is low, the baroreceptors sense the decreased stretch in the blood vessels. It then sends the signal to the Control center in the brian (medulla) to increase the blood pressure by releasing renin.
-Describe the renin-angiotensin system, mentioning the role of renin, angiotensin converting enzyme, angiotensin II, and its effects on PR and its role in stimulating release of both aldosterone and anti-diuretic hormone (ADH).
RAAS -> aldosterone, adh
Renin converts angiotensinogen into angiotensin1, and the ACE converts angiotensin1 to angiotensin2.
Angiotensin2 itself constricts the arterioles which increases blood pressure.
Angiotensin2 also activates ADH and aldosterone.
ADH increases the water reabsorption in the collecting duct by increasing the water permeability toward the membrane, activating more aquaporins.
Aldosterone increases Na+ reabsorption and K+ secretion. Water follows the flow of Na+ by the osmosis, which means Na+ reabsorption also increases water reuptake.
Both ADH and Aldosterone increase the blood pressure by increasing water volume in our body.
It increases Peripheral resistance as the blood flow increases.
PPT
[RBC] homeostasis
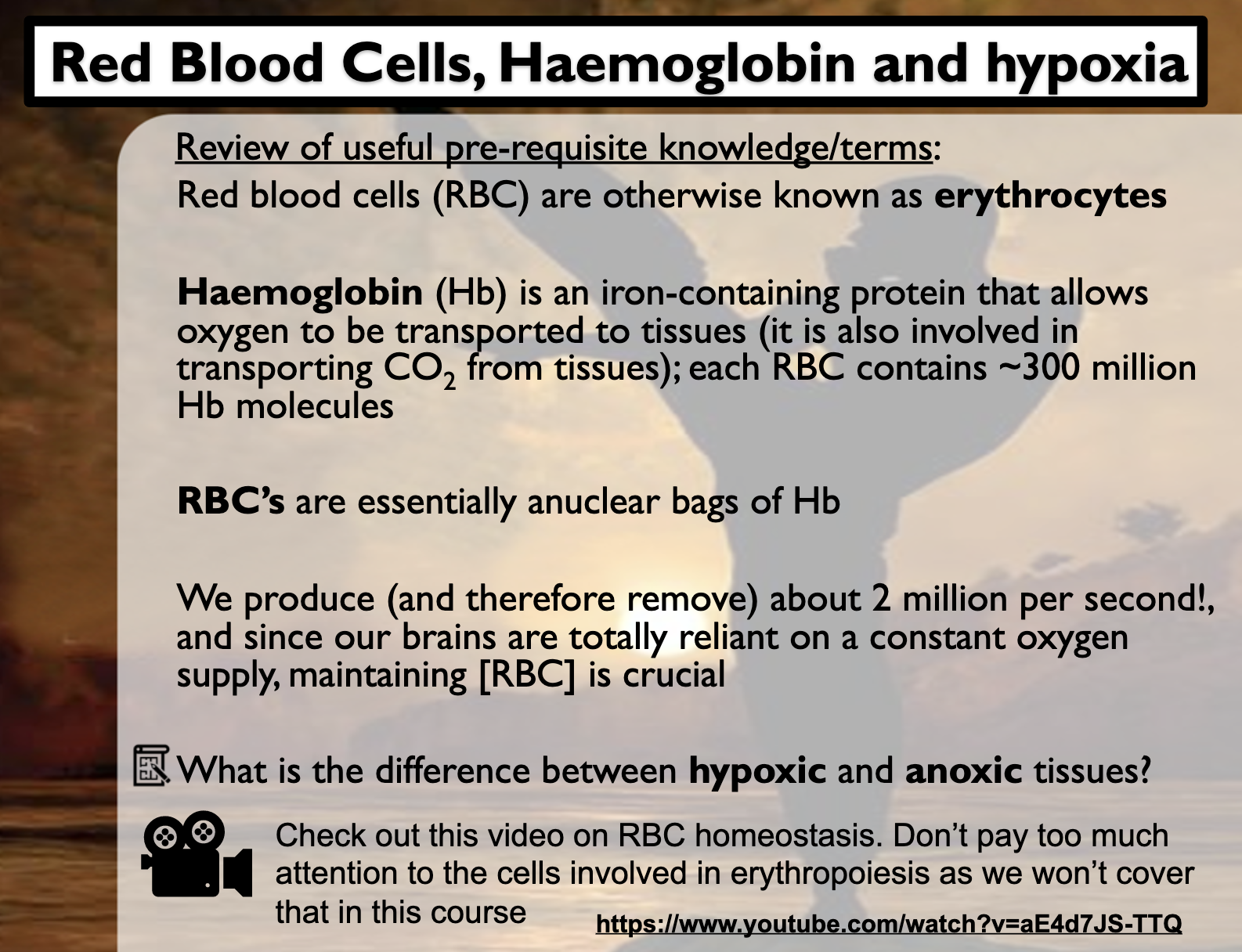
Anoxia is a condition in which there is an absence of oxygen supply to an organ's tissues although there is adequate blood flow to the tissue. Hypoxia is a condition in which there is a decrease of oxygen to the tissue in spite of adequate blood flow to the tissue.
<Role of integrating centers>
-Complex matters such as control of blood pressure and thermoregulation require control over the heart, blood vessels, fluid balance, salt balance etc.
-As a result, the role of the CNS is crucial; there are many inputs and outputs that require coordination
-However, some mechanisms are simpler as the next 3examples indicate - the kidneys are involved in all 3, one way or another, as will become obvious. (water uptake, Ca2+reabsorb, EPO release)
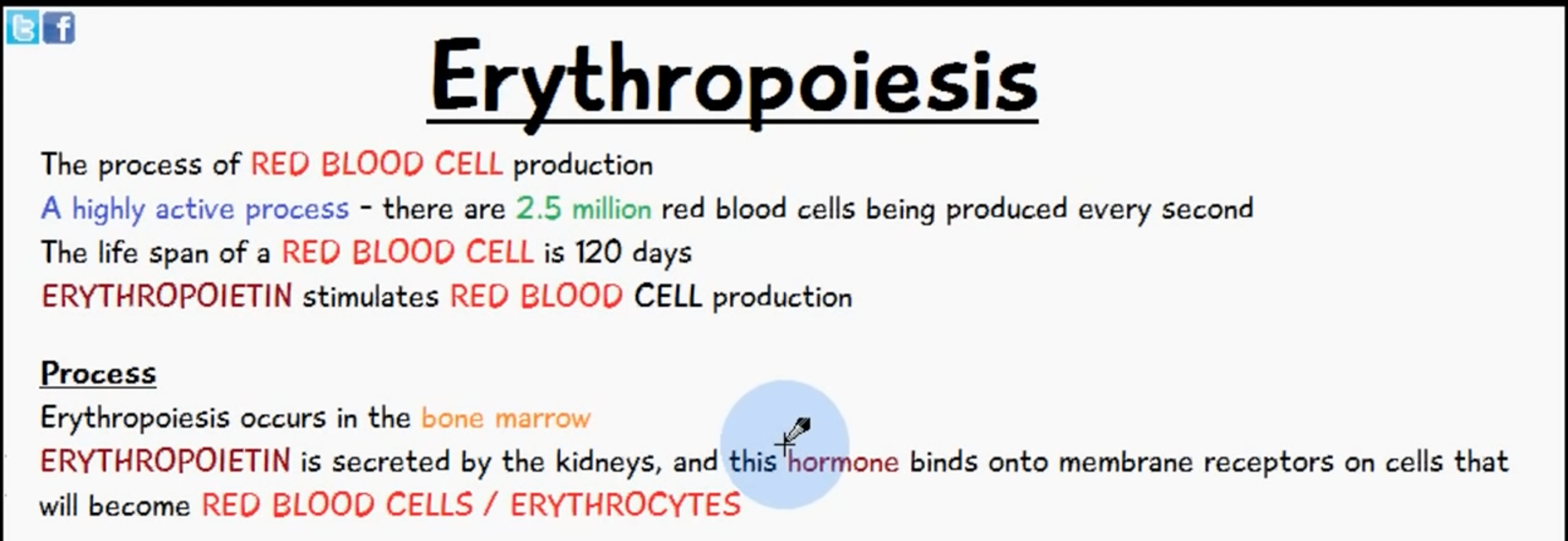
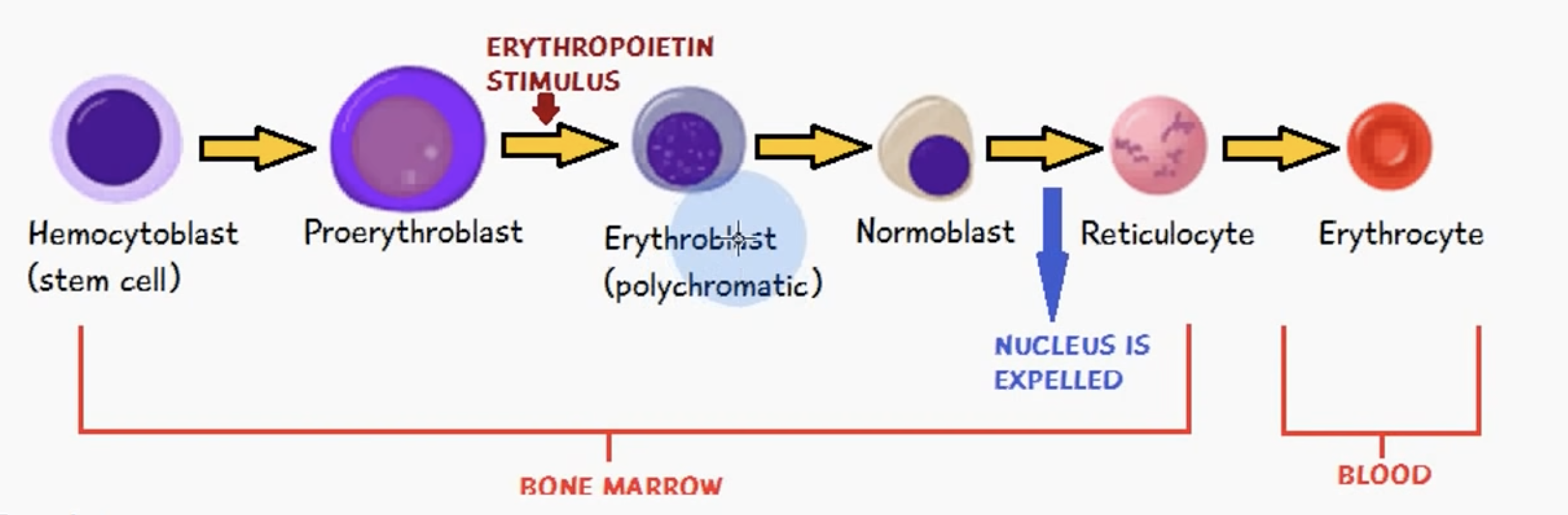
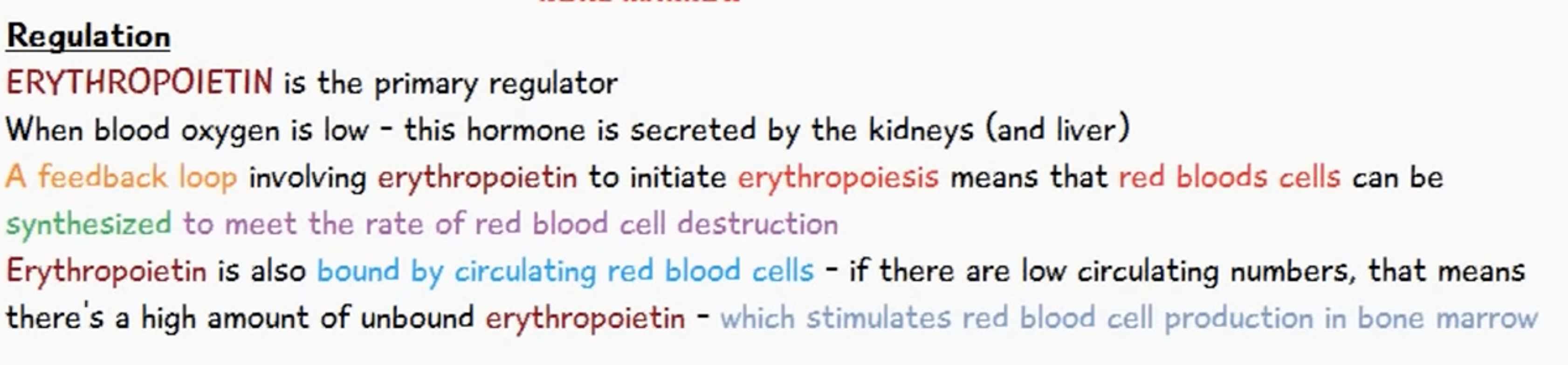
Kidney detects the decreased O2 concentration level and the amount of RBCs in the blood.
It produces erythropoietin, which stimulates erythrogenesis in the red marrow of the bone.
Erythrogenesis refers to the process of producing red blood cells, erythrocytes.
Hemoglobin in the RBC increases the O2 concentration in the blood.
It negates the stimulus to produce erythropoietin in the kidney.
There's no control center in the control of RBC, and the sensor and the effector are both kidney.
Calcium Homeostasis
<Role of Calcium in the body>
: Blood [Ca2+] must be maintained within tolerable ranges because..
-Very many metabolic roles of Ca2+ are crucial to life (eg. Heart contraction, nerve action, blood coagulation, cell division..)
-And as a result Ca2+ will be taken off bone if blood levels are low, with little regard as to how strong the bones are to begin with… what might result from this? osteoporosis
-Osteoclasts resorb bone to release calcium (and phosphate, inadvertently), while osteoblasts remove calcium from blood to build bone.
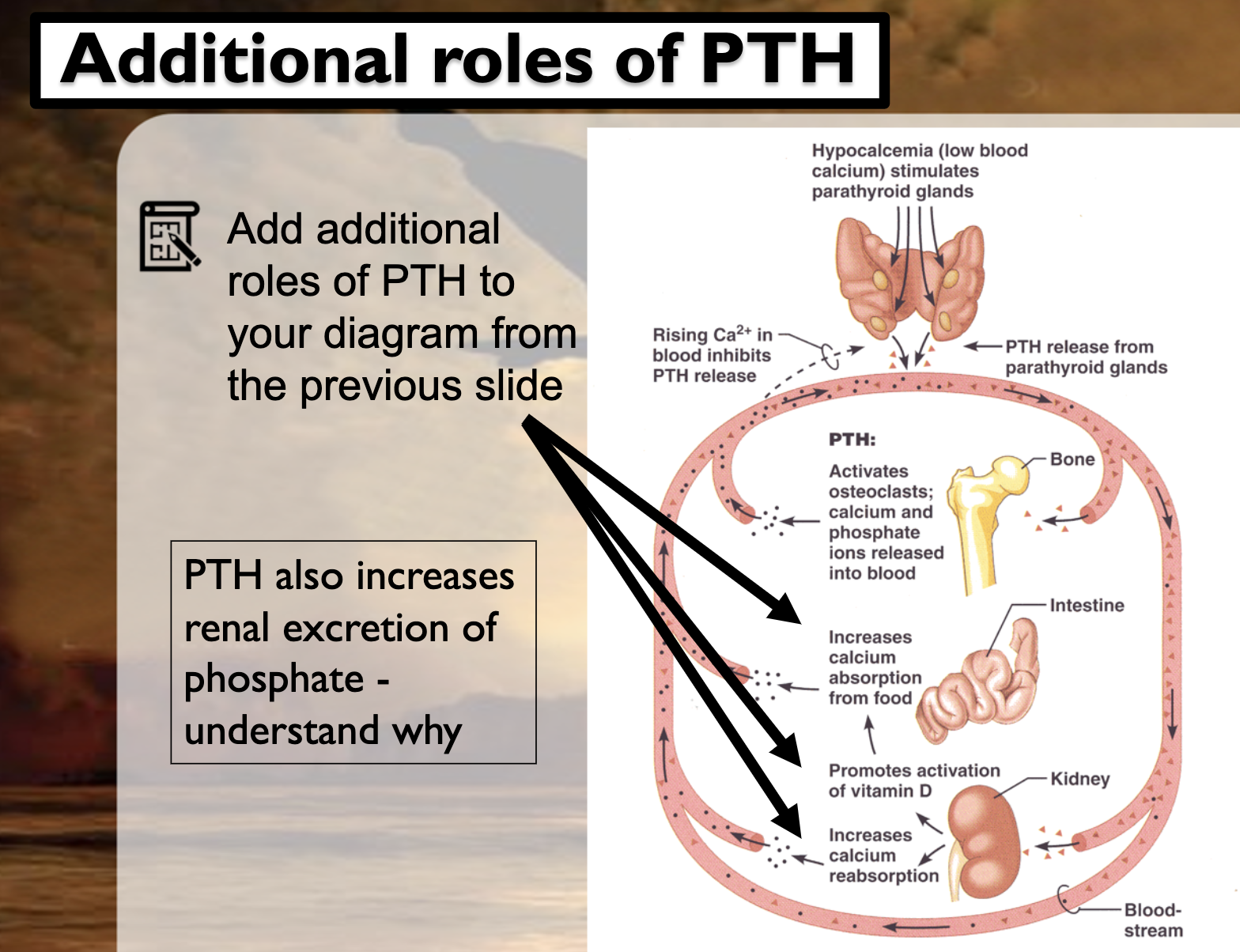
-What function is for PTH increasing renal excretion?
PTH activates osteoclasts to break down the bone to release Ca2+ into the blood. It also stimulates the kidney to increase reabsorption of the Ca2+. Kidney also activates the vitamin D, which increases Ca2+ absorption in the intestine.
PTH increases renal excretion of phosphate. If there's high concentration of phosphate in the blood, it forms Calcium phosphate by reacting with calcium. Calcium phosphate is insoluble salt, and it decreases calcium concentration in the blood.
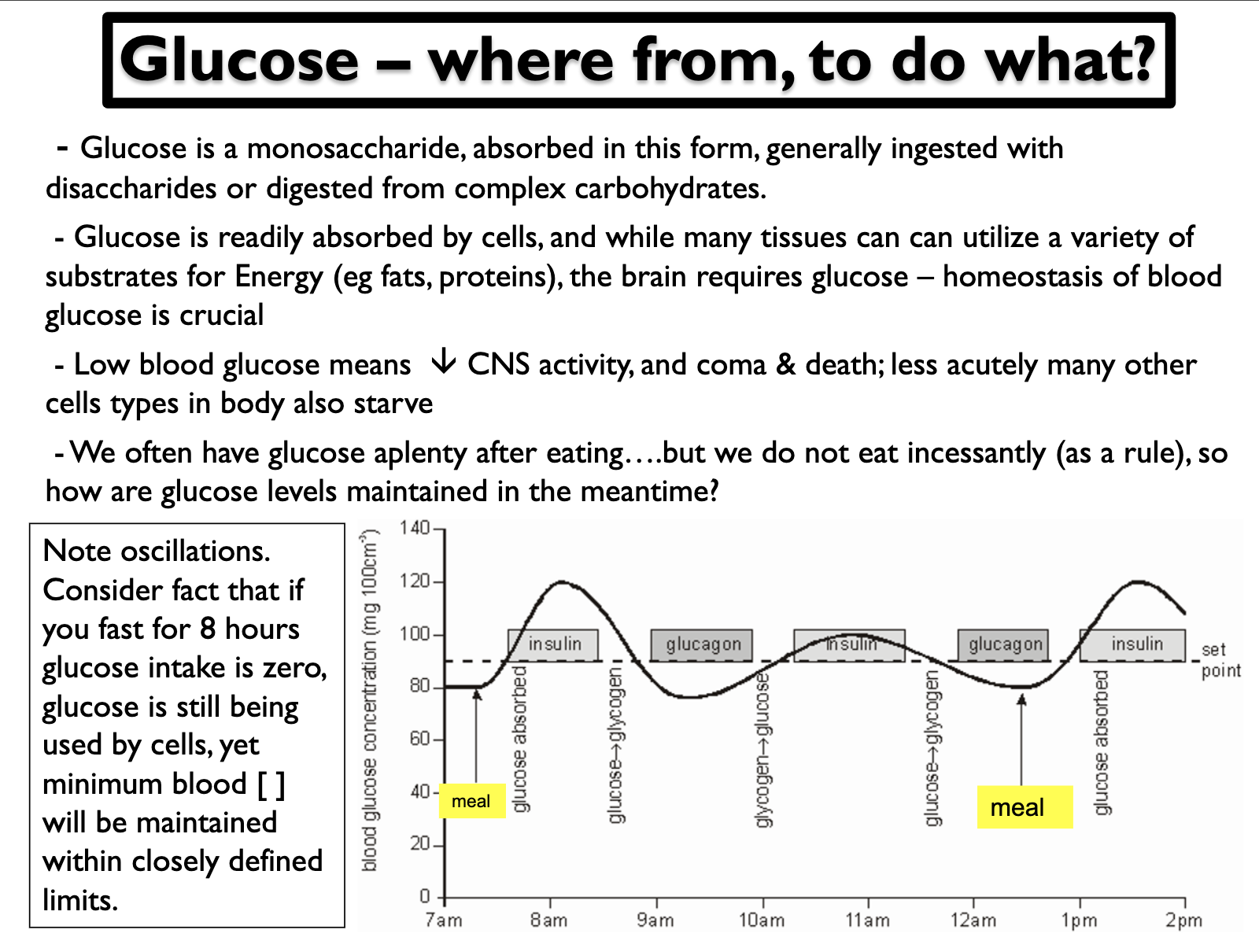
Glucose Homeostasis
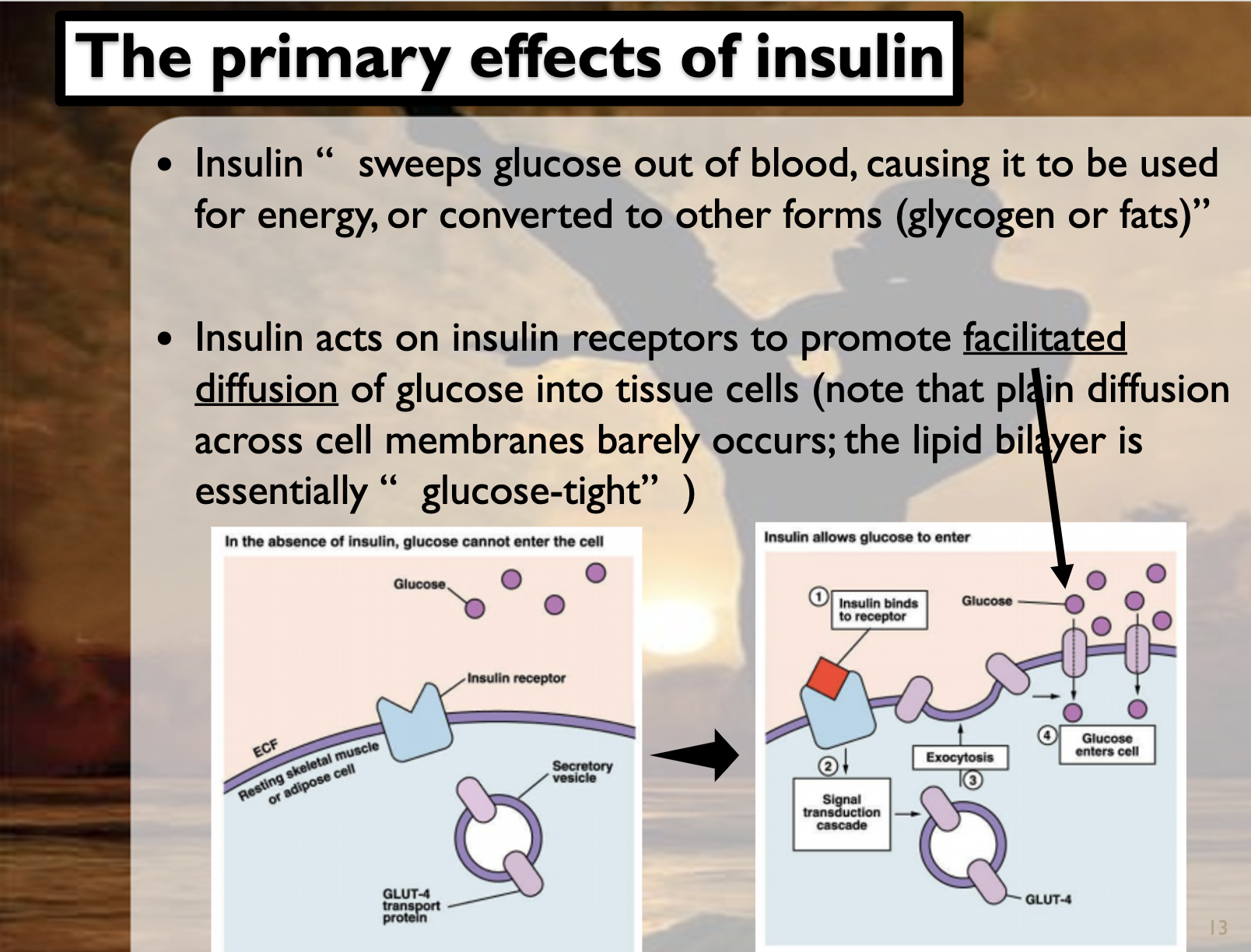
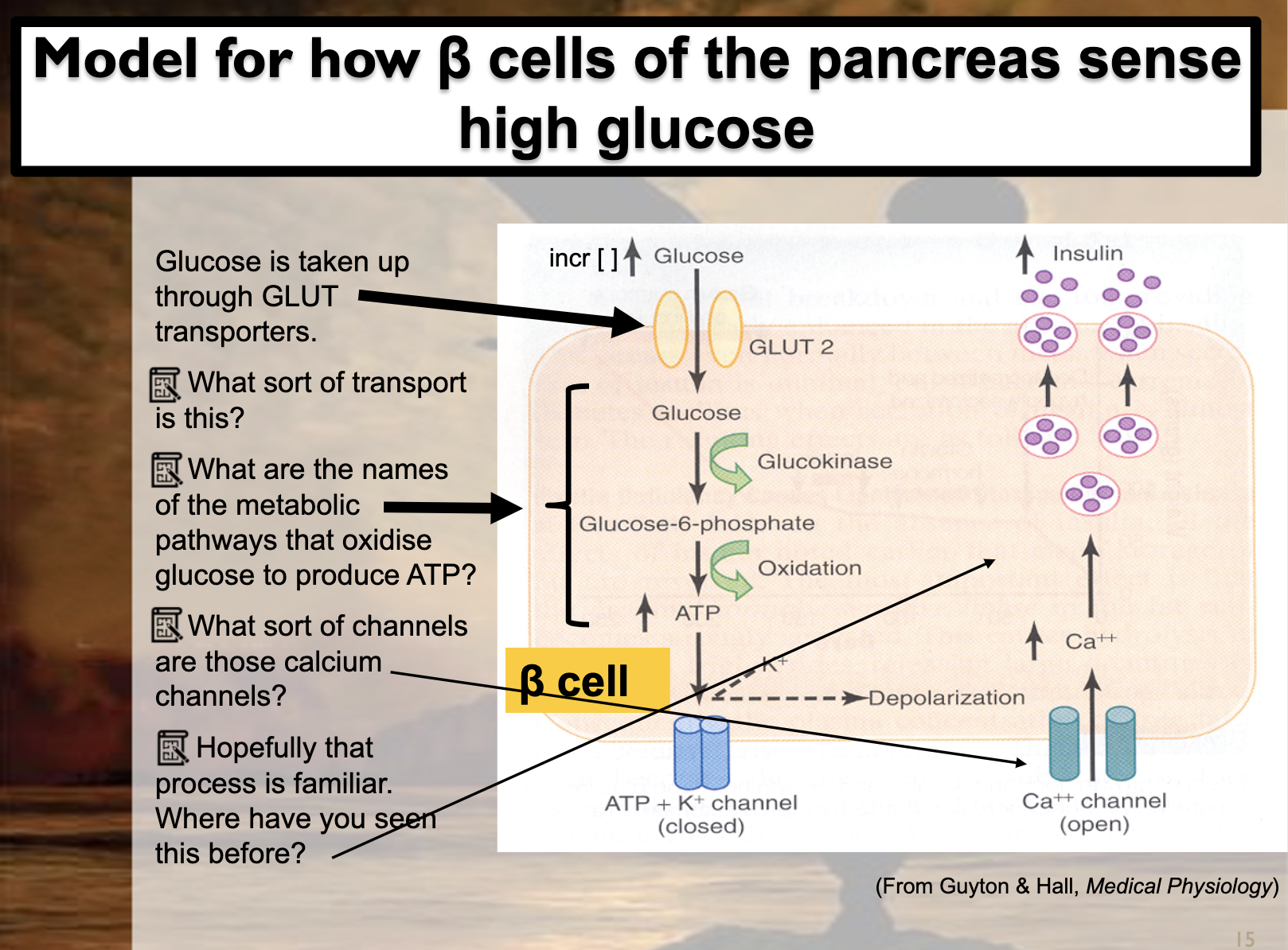

The glucose transporter GLUT4 is critical for skeletal muscle glucose uptake in response to insulin and muscle contraction/exercise. Exercise increases GLUT4 translocation to the sarcolemma and t-tubule and, over the longer term, total GLUT4 protein content.
<Diabetes mellitus - choronic consequences>
: Regardless of aetiology, diabetes mellitus is leading cause of
-blindness
-amputation of lower limbs
-kidney failure
-impotence 무력
-cardiovascular disease (high blood fats)
-acidosis (loss of control over pH, can’t burn glucose, Energy from burning of fats, = ketoacidosis, can be acutely life threatening)
-The result of a range of metabolic anomalies, including damage to small blood vessels and nerves, high blood fats, and excessive glucose altering biochemical processes.
<Blood [glucose] overview>
1. How a crucial variable is monitored and controlled within the body without much input from the CNS
2. That diabolical consequences, both acute &choronic, occur once homeostatic control over a crucial variable is lost
<Diabetes insipidus>
-This condition is rare, has nothing to do with loss of control over blood [glucose], but like DM does cause a diuresis
-DI results when there is inability to concentrate urine, and the resultant diuresis may be 3-15L/day ! However, provided [electrolyte]’s maintained & there is sufficient water intake, suffers can be quite stable.
(Causes)
-Neurgenic : insufficient prod/release of ADH from post-pituitary.
Often due to hypothalamic tutors, or damage due to head trauma.
-Nephrogenic : often seen in end-stage kidney disease, cells no longer receptive to ADH
-Psychogenic : vastly increased H2O intake in mentally disabled or health freaks (mutually exclusive?) -can drink themselves to death (water intoxication)
Blood pressure Homeostasis
<How crucial is BP control?>
-BP homeostasis is critical, tolerances are low, particularly with respect to acute falls in BP
-BP control, like that of thermoregulation, requires extensive CNS integration
-Baroreceptors are stretch receptors; less stretch with falling BP stimulates cardiac control centers in the brain to activates the SNS to increase BP- what sort of gates are baroreceptors ion channels likely to have? mechanically gated ion channels
-Result: CO & PR(pulse rate,heart rate) both increased- do you think that all arterial vessels constrict in order to increase PR? -no, some arterials are constricted and some are not. It controls them effectively
-Triggers to increase blood volume also occurs via SNA stimulation of renin release
<The end of homeostasis>
-We have discussed 5 homeostatic systems
: thermoregulation, blood [rbc], blood [Ca2+], blood [glucose] and blood pressure. And in emphasising the role played by the kidneys overall also partially dicussed homeostasis of fluid and salt balance
-> sympathetic nerves, afferent & efferent signals, osmosis, active transport, facilitated diffusion, hormones, receptors, including receptrs up-regulation, down regulation,… all of these important entities described earlier in CTR are incorporated in explanations of how homeostatic mechanisms work
-There is much more to learn including details on control over BP (complex interconnecting paths), and control over pH(which is acutely crucial; kidneys play a major role)
-The principles remain; there are sensors, integrating centers, negative feedback loops and effectors
-If you are to understand human physiology, you must understand these common principles, and be able to describe specific homeostatic mechanisms, in some detail
Homeostatic mechanisms are operated by stimulus, sensor, integrating centers(not always), effectors, and negtive feedback loops. The stimulus makes the variable around the setpoint, which is called osciliation. Within the normal range of the body function, when the variable hits the bottom of the level, negative feedback loop operate and control the negate the deviation.
Self paced quiz
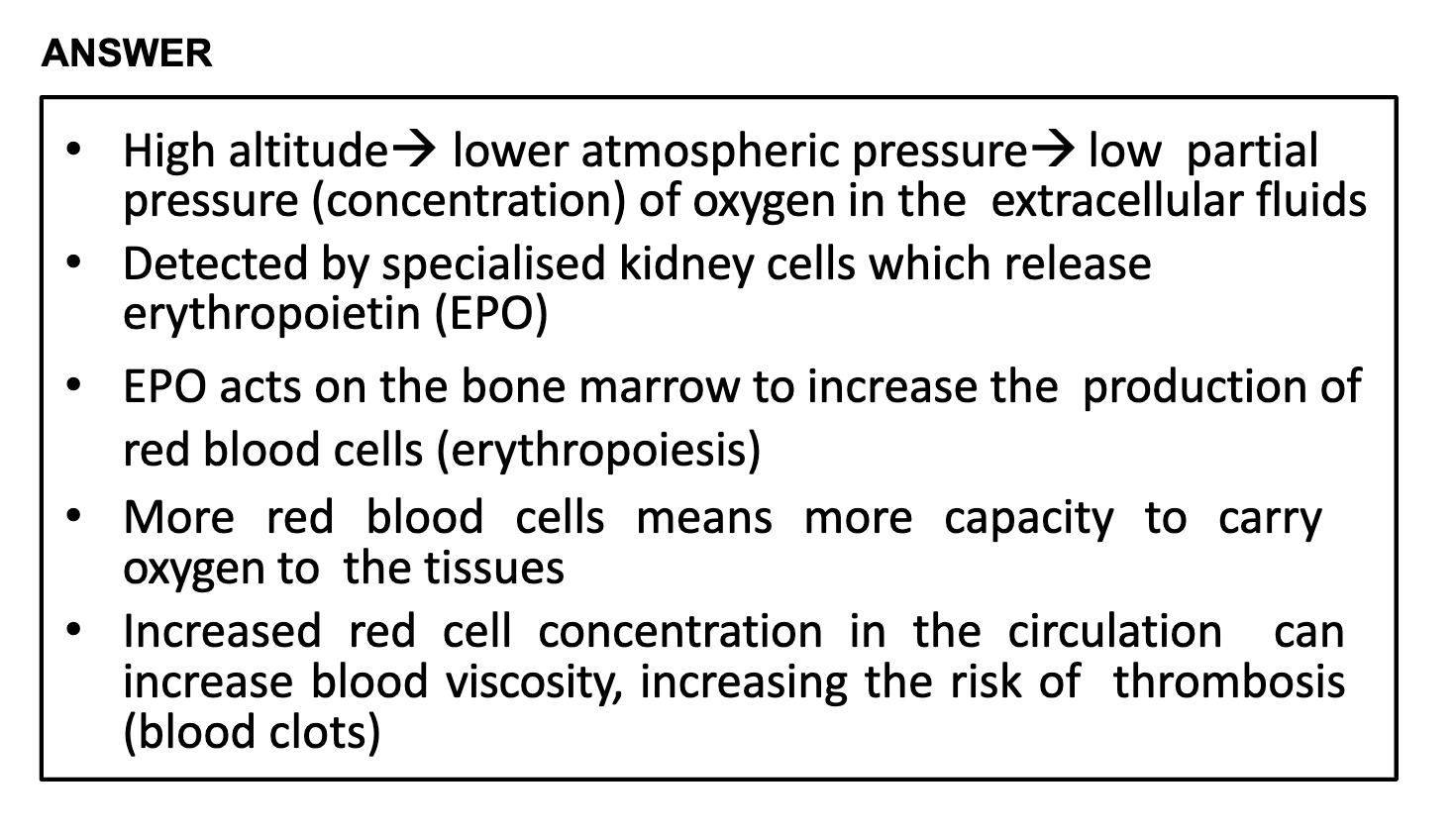
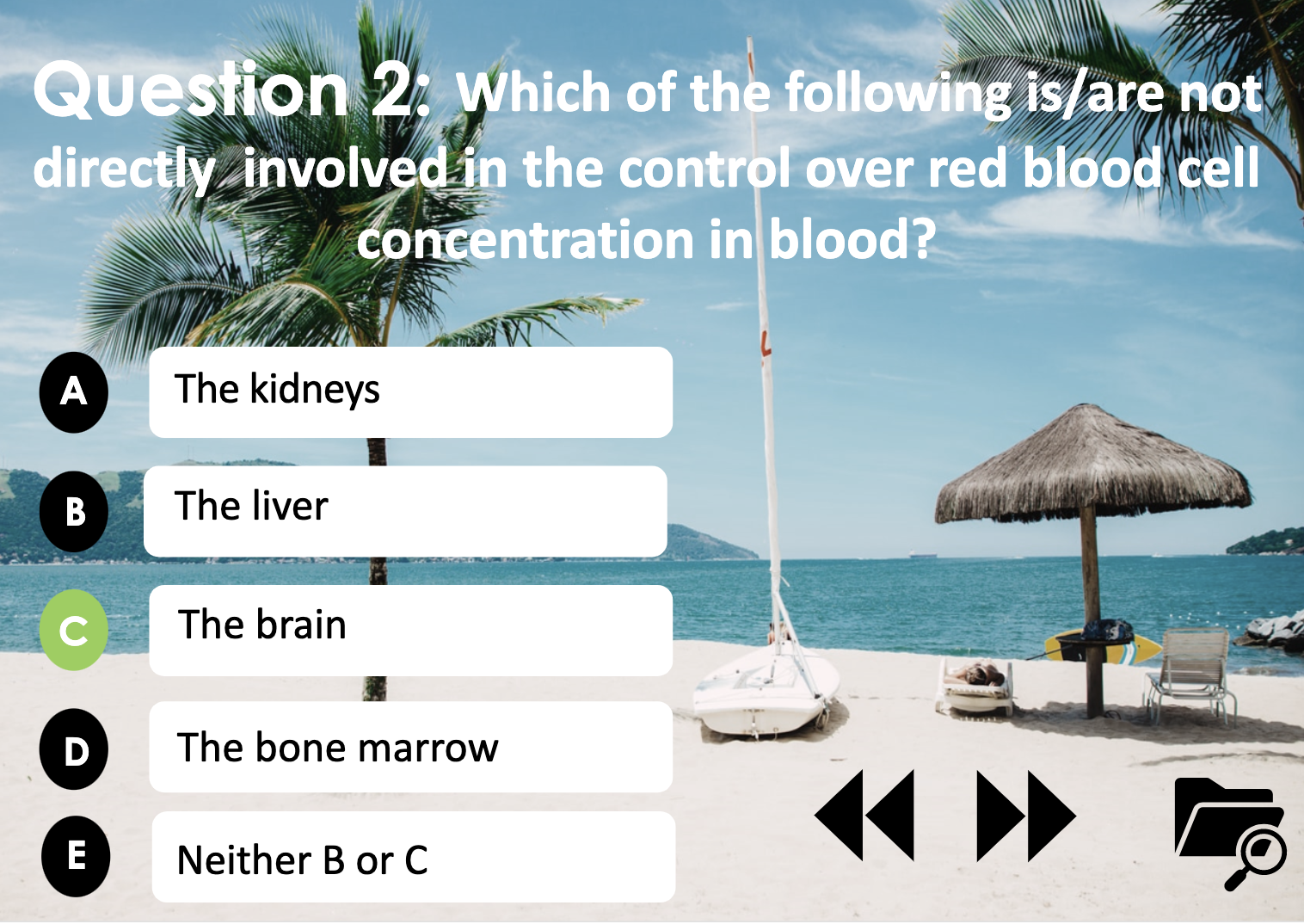
The red bood cell concentration would increase. Because the Andes environment lacks of oxygen, our body will produce more RBC to increase the delivery of oxygen. The cell in the kidney detect the need of producing more RBC, it releases erythropoietin(EPO), which binds to the erythroblast which becomes to RBC (erythropoiesis). However, too much RBC in the blood can result in increasing blood visocity, which can thichken the blood, slow flow of blood and eventually blood clots.
Liver and RBC
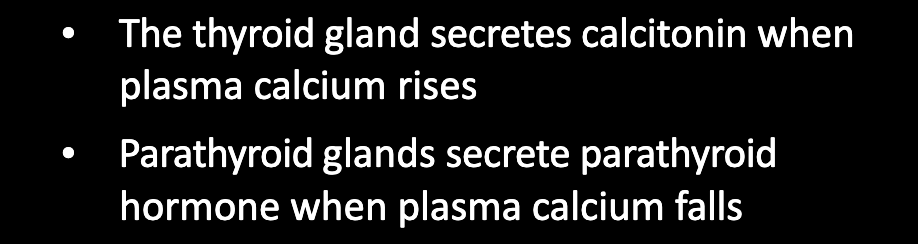
Parafollicular cells in Thyroid gland produces calcitonin, which decreases Ca2+ level in the blood. Parathyroid gland releases parathyroid hormone which increases osteoclasts activity and reabsorption of Ca2+ in kidney and intestine, which in turn increases Ca2+ level in blood.
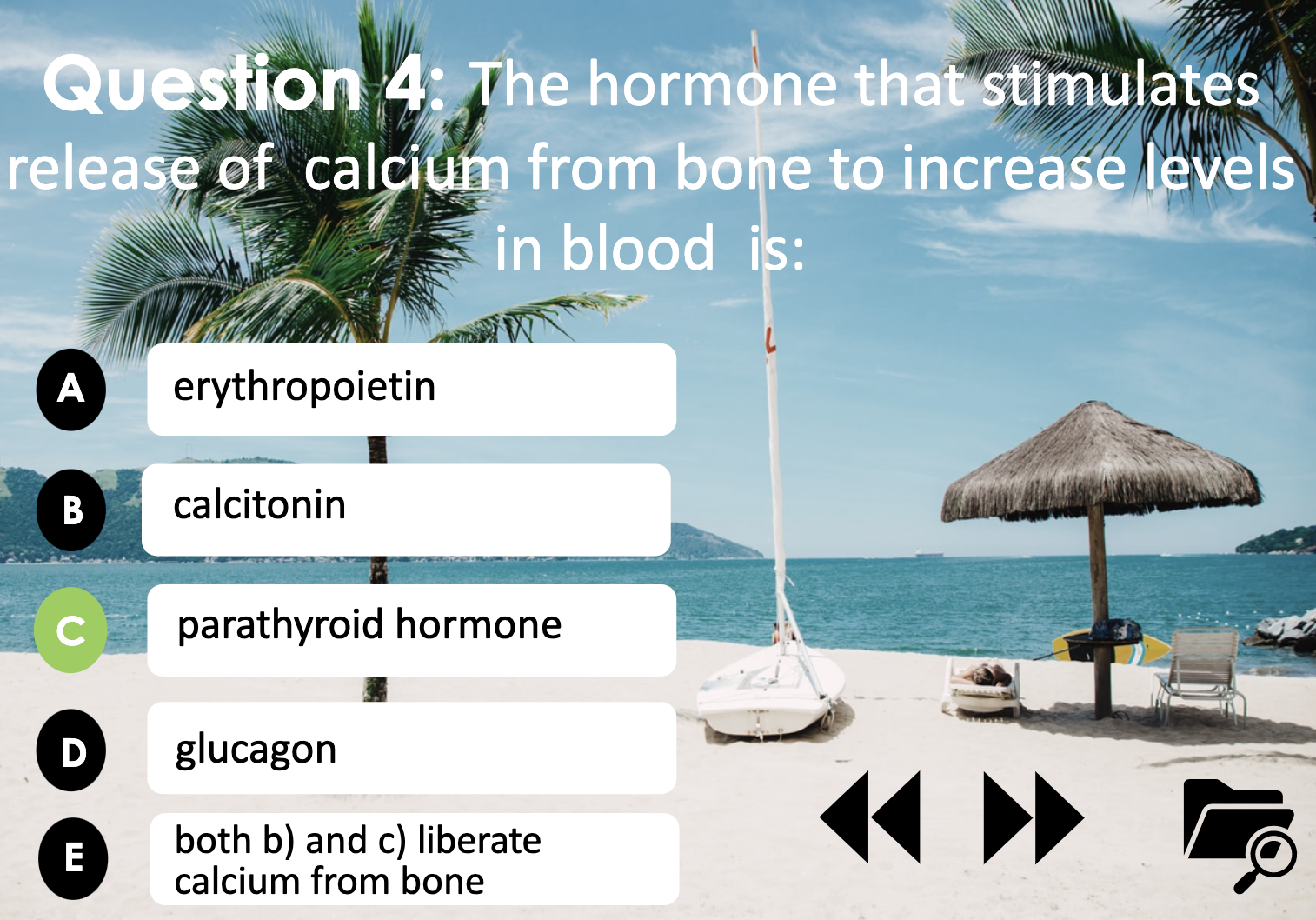
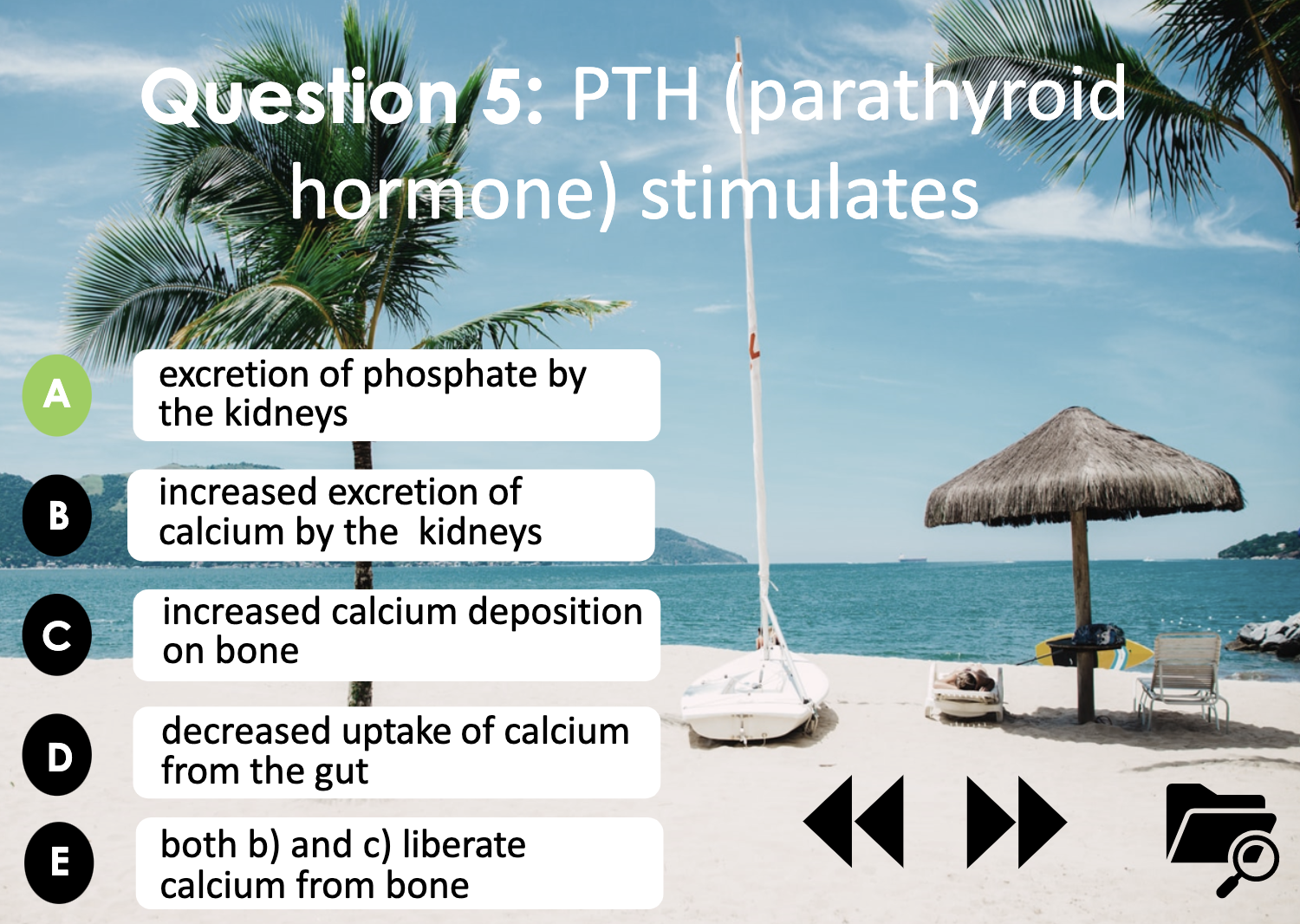
PTH and Phosphate
PTH stimulates kidney to excrete phosphate. Phosphate reacts with calcium ion to make Calcium phosphate, which deposits in the bone and strengthen it, which doesn't help in increasing the Ca2+ level in blood.
PTH increases renal excretion of phosphate. If there's high concentration of phosphate in the blood, it forms Calcium phosphate by reacting with calcium. Calcium phosphate is insoluble salt, and it decreases calcium concentration in the blood.
Insulin's glucose control
Insulin is secreted to decrease the blood sugar(glucose) level. It combines to the receptors in the tissue cell membrane. The receptor send the signal to start the cascade, which activates GLUT 4 transport protein. GLUT 4 exocytosis and enables facilitated diffusion of glucose. The glucose molecule cannot enter into the tissue cell directly because the membrane is lipid soluble and the glucose is water soluble.
Insulin generates glycogen from glucose, which is an anabolic reaction. It needs energy to synthesize bigger compound. Insulin inhibits aminoacids and lipid to produce glucose.
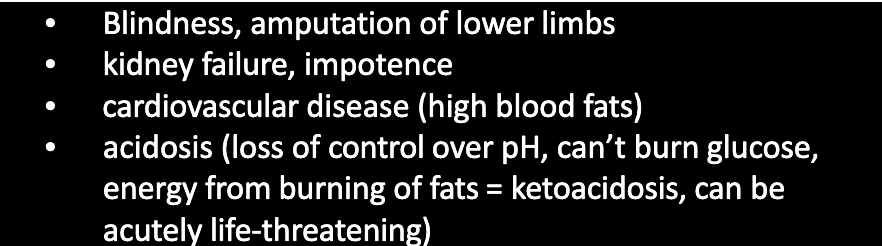
-blindness
-amputation of lower limbs
-kidney failure
-impotence 무력
-cardiovascular disease (high blood fats)
-acidosis (loss of control over pH, can’t burn glucose, Energy from burning of fats, = ketoacidosis, can be acutely life threatening)
-The result of a range of metabolic anomalies, including damage to small blood vessels and nerves, high blood fats, and excessive glucose altering biochemical processes.
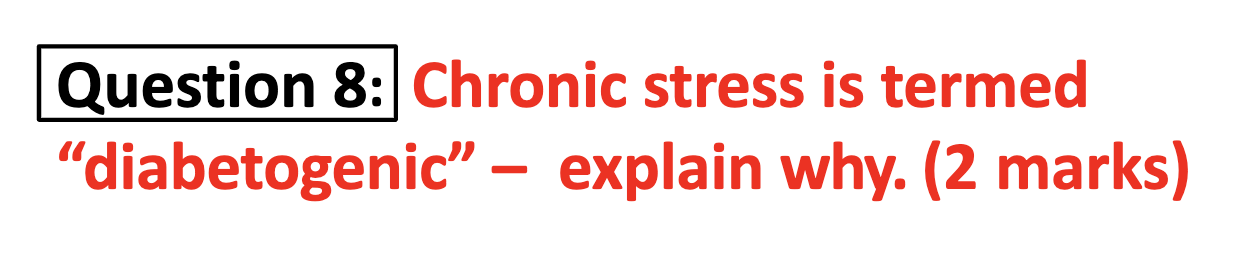
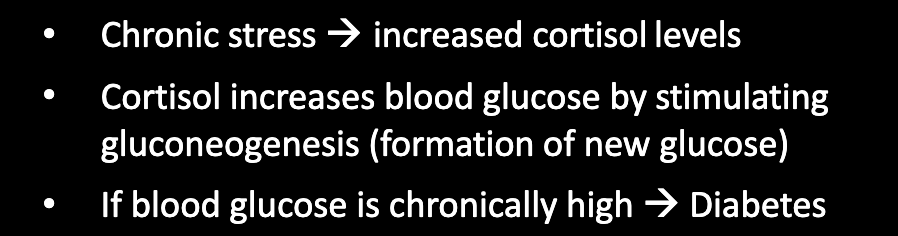
Stress - diabetogenic
Stress acts as a stimulus for increasing cortisol level. When cortisol is secreted from the adrenal cortex, it activates glucogenesis in the liver, which increases blood glucose level. Diabetes refers to the condition when there's high glucose level in the blood. When the stress becomes choronic, cortisol will increase glucose level in blood stream continuously and it can seem as diabetes, which is termed diabetogenic.

<Diabetes insipidus> ADH decrease, Nephron's ADH receptors damaged, H2O intake increases
-This condition is rare, has nothing to do with loss of control over blood [glucose], but like DM does cause a diuresis
-DI results when there is inability to concentrate urine, and the resultant diuresis may be 3-15L/day ! However, provided [electrolyte]’s maintained & there is sufficient water intake, suffers can be quite stable.
(Causes)
-Neurgenic : insufficient prod/release of ADH from post-pituitary.
Often due to hypothalamic tutors, or damage due to head trauma.
-Nephrogenic : often seen in end-stage kidney disease, cells no longer receptive to ADH
-Psychogenic : vastly increased H2O intake in mentally disabled or health freaks (mutually exclusive?) -can drink themselves to death (water intoxication)
When I leap out of bed, Blood pressure in brain suddenly hits down and it causes the feeling of faint. The brain detects the slight decrease in the blood flow as the blood flows toward the leg.
(short term of BP increase)
Increase in cardiac output and peripheral resistance can correct this problem quickly by the sympathetic nervous system.
When the baroreceptor detects the vasodilation, it sends the signal to the vasomotor center in the brain (medulla) and the center sends the signals to the heart and the smooth muscle in the blood vessels.
In the heart, activated cardiac output helps the blood pressure increase, and in the blood vessels, peripheral vasoconstriction prevents the blood from flowing toward the leg so that the blood flow doesn't lack in the brain.
(Long term of BP increase)
Unlike to the sympathetic nervous system increasing cardiac output and peripheral resistance, for long term control, kidney is involved. Kidney activates RAAS, starting with releasing renin from the renal cells. Renin activates angiotensin2, which constrict blood vessels. It also activates aldosterone and ADH , which increase BP by reuptaking Na+ and water, in the distal convoluted tubule and collecting duct respectively. (ADH has also the function of constricting the blood vessel as it has alternative name vasopressin)

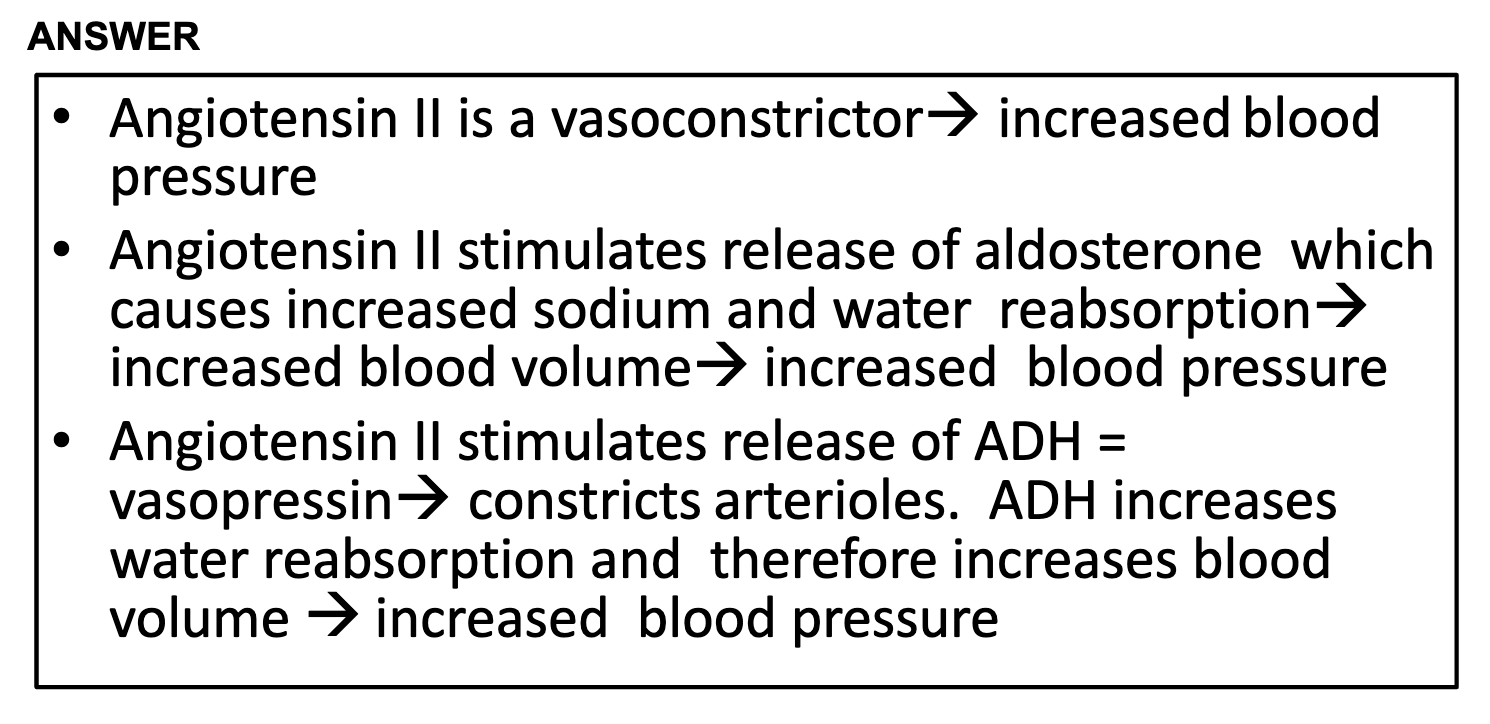
Renin converts angiotensinogen into angiotensin1, and the ACE converts angiotensin1 into angiotensin2.
Angiotensin2 itself constricts the arterioles which increases blood pressure.
Angiotensin2 also activates ADH and aldosterone.
ADH increases the water reabsorption in the collecting duct by increasing the water permeability toward the membrane, activating more aquaporins.
Aldosterone increases Na+ reabsorption and K+ secretion. Water follows the flow of Na+ by the osmosis, which means Na+ reabsorption also increases water reuptake and in turn blood pressure. (in the distal tubule of nephron)

Blood pressure is monitored by the baroreceptors in the blood vessels. Baroreceptors are mechanoreceptors ,which have mecahnically gated channels, sense the pressure, and stretch as the stimulus.
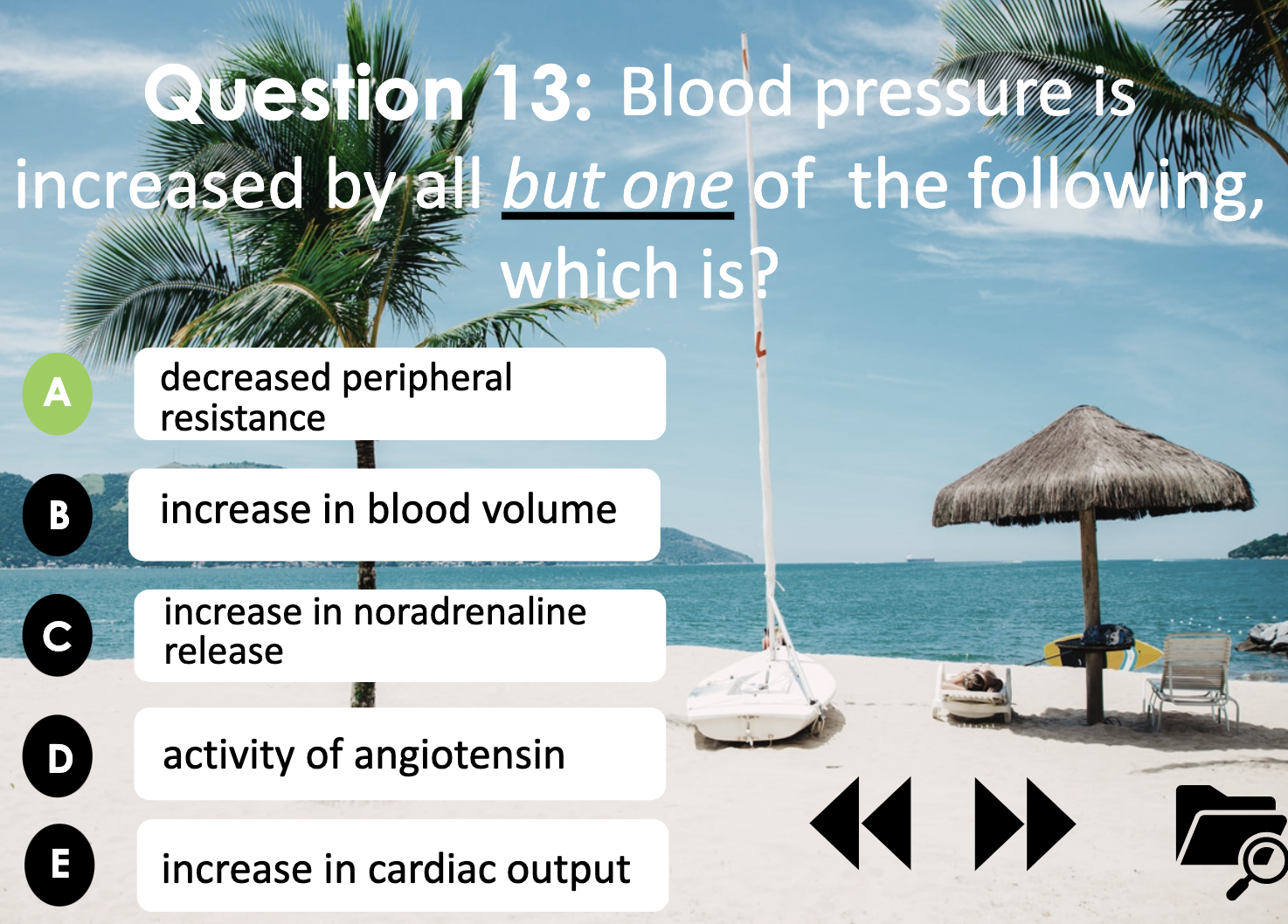
<Blood pressure increased by..>
- increased peripheral resistance ( but not ALL the blood vessels in peripheral constricts to be efficient)
: vasoconstriction makes the blood pressure increase
-increase in cardiac out put
: Baroreceptor send the signal to the brain vasocontrol center. It then send the signal to the heart to increase cardiac output, which increase heart beat and blood pressure.
-increase in blood volume
: ADH, aldosterone increases the water retention and it makes the blood pressure increase.
-increase in noradrenaline release
: sympathetic nervous system -> neural stimulus to adrenal medulla to secrete noradrenaline.
Noradrenaline binds to the a receptors which results in constriction of blood vessels. -> blood pressure increase
-activity of angiotensin
: angiotensin2 constricts the blood vessels. It also stimulates the ADH and aldosterone to increase blood pressure by activating kidney to reabsorb more water.
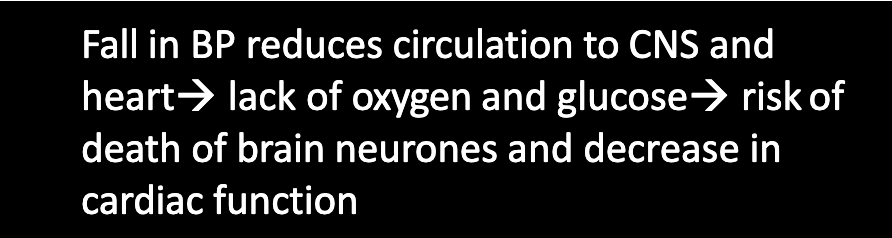
The immediate problem is caused by a fall in blood pressure. It reduces the blood flow to CNS and heart, which results in damaging brain neurons and cardiac function.
'Griffith college Tri3 2022 > 1014MSC (CTR)' 카테고리의 다른 글
| WEEK 11, 12 - Questions and Answers from Homeostasis summary (0) | 2023.01.15 |
|---|---|
| WEEK11 - module 4. Physiological examples of homeostasis (0) | 2023.01.05 |
| WEEK10 - module 4. Principles of Homeostasis (0) | 2022.12.22 |
| WEEK9 - module 3. Endocrinology (0) | 2022.12.15 |
| WEEK8 - module 3. The Synapse (0) | 2022.12.09 |



